Peripheral Blood Stem Cell Transplant (PBSCT) for Cancer
Peripheral Blood Stem Cell Transplant (PBSCT) for Cancer
Peripheral blood stem cells are immature cells. They make white cells, red cells, and platelets. White cells fight infection. Red cells carry oxygen. Platelets prevent bleeding. Some types of cancer treatment damage stem cells. A peripheral blood stem cell transplant (PBSCT) replaces stem cells that have been destroyed by cancer treatment.
How PBSC works
Stem cells are collected before cancer treatment. After treatment, the cells are put into your bloodstream. The cells travel to your bone marrow and begin making new blood cells. Stem cells can be collected from your own blood. This is called an autologous transplant. Or they may come from a donor. This is called an allogeneic transplant. These stem cells may also be able to kill cancer cells and prevent relapse. This is known as the graft-versus-tumor effect. The type of transplant used depends on various factors. Both types have advantages and risks.
Autologous PBSCT
This type of transplant comes from your own stem cells.
-
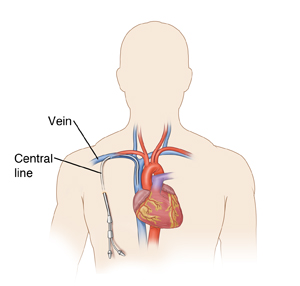
Before the transplant. First, the stem cells are collected (removed from your body) one month to several years before your transplant. A week or so before the stems cells are collected, you will be given medicine to help your bone marrow make more stem cells. Your blood will be tested each day to see if you have enough stem cells to collect. Before collection, a thin, flexible tube called a catheter is placed in a vein in your neck, chest, or groin. This is called a central line. The collection can take one or more days. During this time, you will be connected to a special machine. The machine removes some blood, takes out the stem cells, and returns the blood to you. You may feel a tingling in your lips or hands. The collected stem cells are frozen in a special freezer. Stem cells can be safely stored for many years. Then before your transplant, you will also have high-dose chemotherapy. Or you may have radiation. These procedures are usually done in a hospital or clinic.
-
The transplant procedure. The transplant can be done in a hospital, clinic, or at home. The stem cells are given through your central line into your bloodstream. The procedure can take several hours to a day or more. During the transplant, you may also feel short of breath or have a tight feeling in the chest. You may have high or low blood pressure. A nurse will be with you during the transplant. You will be monitored closely. You will also receive IV (intravenous) fluids. This helps wash out a preservative called DMSO that is used to store the stem cells. DMSO may cause a taste or smell like garlic or creamed corn. You will notice this during the stem cell transplant and up to 36 hours later.
Allogeneic PBSCT
This type of transplant comes from donor stem cells.
-
Before the transplant. You will receive chemotherapy. This may be high-dose therapy that kills the cells in your bone marrow. This is called myeloablative therapy. Or it may be lower-dose chemotherapy. The type you have depends on certain factors. Your doctor can tell you which you will have. You may also receive radiation. These procedures are usually done in a hospital or clinic.
-
The transplant procedure. The stem cells are usually transplanted the day after the last dose of chemotherapy. The donor cells are given “fresh.” This means they have not been frozen and don't contain preservatives. The stem cells are given through your central line into your bloodstream. The procedure can take several hours. During the transplant you may also feel short of breath or have a tight feeling in the chest. You may have high or low blood pressure. A nurse will be with you during the transplant. You will be monitored closely. You will also receive IV fluids.
Recovering at Home
Once you return home, follow the instructions you have been given for caring for yourself. These include:
-
Take all medicines as directed. You will be given medicine to help prevent infection. If you had an allogeneic transplant, you will take medicine to prevent graft-versus-host disease (GVHD). This is a reaction between the donor stem cells and your body. You may need to take these medicines for up to 1 year.
-
Care for your central line as instructed. Proper care helps prevent serious infection. Avoid swimming and hot tubs while you still have your central line.
-
Avoid people with colds, flu, or other contagious illness until your blood counts have returned to normal.
-
Be aware that depending on your type of transplant, you may need to avoid some high-risk activities such as gardening for up to 1 year. Discuss this with your healthcare provider.
-
Take care to avoid germs and molds that may make you sick. Make sure your food is well cooked. Handle food only with clean hands. Don't change litter boxes. Wash your hands often to prevent infection.
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
-
Fever of 100.4ºF (38ºC) or higher, or as directed by your healthcare provider
-
Chest discomfort or pain
-
Trouble breathing
-
Coughing
-
Ongoing fatigue
-
Headache
-
Nausea or vomiting
-
Diarrhea
-
New or worsening skin rash
-
Bruising or bleeding
-
Urinating less than usual
-
Severe fatigue (tiredness)
-
Any other signs or symptoms indicated by your doctor
Updated:
March 15, 2019
Reviewed By:
Freeborn, Donna, PhD, CNM, FNP,LoCicero, Richard, MD