Mastectomy with Reconstruction
Mastectomy with Reconstruction
Mastectomy is surgery to remove a breast. It’s most often done to treat breast cancer. Or it may be done to keep cancer from spreading. After a mastectomy, reconstruction can be done to rebuild the breast shape and restore its appearance. Reconstruction is done using either breast implants or tissue from another part of the body (flap reconstruction). The tissue can come from the belly, buttocks, inner thigh, or back. Mastectomy and reconstruction may be done at the same time. Or they may be done separately, so your body can heal in between. This sheet explains the surgeries and what to expect.
Getting ready for surgery
Prepare for surgery as you have been told. In addition:
Tell your healthcare provider about all medicines you take. This includes prescription medicines, over-the-counter medicines, herbs, vitamins, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery.
Follow any directions you are given for not eating or drinking before your surgery. This includes coffee, water, gum, and mints. If you have been instructed to take medicines, take them with a small sip of water.
The day of surgery
When the surgeries are done together, mastectomy is done on one or both breasts, followed by reconstruction. When the surgeries are done separately, mastectomy is done on one or both breasts, with reconstruction scheduled for a later date. Surgery may take 2 to 12 hours depending on your situation. Ask your surgeon how long your surgery is expected to take. You will stay for 1 or more nights in the hospital.
Before surgery begins
An IV (intravenous) line is put into a vein in your arm or hand. This is used to give you fluids and medicines.
Medicine is given so you don't feel pain during the surgery. This may be general anesthesia, which puts you into a deep sleep during the surgery. (A tube may be inserted into your throat to help you breathe.) In some cases, sedation is used instead. This makes you relaxed and sleepy. With sedation, local anesthesia will be injected to block the nerves in your chest and prevent pain.
During mastectomy
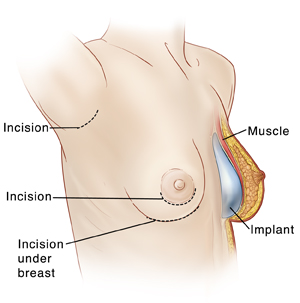
One or more cuts (incisions) are made. In most cases, all of the breast tissue, the skin over the breast, and the nipple are removed. Some of the chest muscles beneath the breast may also be removed.
Lymph nodes near the tumor may be removed and checked for cancer. (Lymph nodes are small masses of tissue that are part of the body’s immune system.) If any lymph nodes contain cancer, other treatments are likely needed after the surgery.
During reconstruction
For breast implants, a sac filled with gel or saline (saltwater) is inserted to re-form the shape of the breast. The implant is usually placed under the chest muscle. If you don’t have enough muscle and skin to cover an implant, you may need a tissue expander. This is an empty implant that is slowly inflated over time. If this is needed, your healthcare provider will tell you more about it.
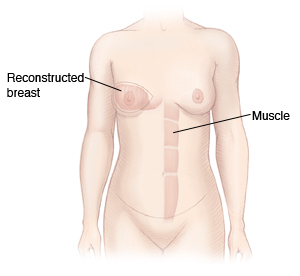
For flap reconstruction, tissue is often taken from the belly (abdominal wall) to rebuild the breast shape. Or the tissue could be taken from other parts of your body. This method is sometimes combined with an implant. Flap reconstruction means you will have 2 surgical sites: the chest and the part of your body where the flap was taken.
With either reconstruction method, a nipple and the area around the nipple (areola) may be built during or after the surgery.
One or two soft plastic tubes (drains) are inserted near the incisions. These help to drain excess fluid that can build up during healing. The incisions are then closed and bandaged.
After the surgery
You will be taken to a room to wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. You’ll be given medicine to manage any pain. Tell your healthcare providers if your pain is not controlled. When you’re ready, you’ll be moved to a room to stay for 1 or more nights. Before you leave the hospital, your healthcare team will show you how to care for your bandages and drains. When it’s time to go home, you will need an adult family member or friend to drive you home. Prepare to have someone stay with you for the first few days, to help at home while you heal.
Recovering at home
Once you are home, follow any instructions you are given. Your healthcare provider will tell you when you can return to your normal routine. During your recovery:
Take any prescribed pain medicine exactly as directed. Good pain control allows you to move and take deep breaths to speed your recovery.
Care for your incisions and the bandage (dressing) over them as instructed by your healthcare provider. Remember, if you have flap surgery you will have 2 surgical wounds: the chest and the part of the body the flap was taken from.
Follow your healthcare provider’s guidelines for showering. Don't swim, bathe, use a hot tub, or do other activities that would cover the incisions with water. Wait until your healthcare provider says it’s OK.
When you shower, gently wash your incision sites. Then pat the incisions dry. Don’t apply lotions, oils, or creams to the incisions until after they are fully healed.
Don’t drive until you are no longer taking prescription pain medicine and your healthcare provider says it’s OK (at least 10 days). When riding in a car, carefully position the seatbelt so that it doesn’t squeeze your breasts.
Care for your drains as directed. They may need to be emptied at least every 8 hours.
If advised by your healthcare provider, use a cold pack to relieve mild pain and control swelling. It’s important not to leave the cold pack on for too long, or your skin could be damaged. Put the pack over your bandages for no more than 20 minutes at a time. Then, leave it off for at least 20 minutes. Repeat this as often as needed during waking hours until swelling starts to improve. Don’t fall asleep with the cold pack on. To make a cold pack, put ice cubes in a plastic bag that seals at the top. Wrap the bag in a clean, thin towel or cloth. Never put ice or a cold pack directly on the skin. If you’re not sure how to safely use the cold pack, ask your healthcare provider.
Walk as often as you feel able.
Don't lift anything heavy or do housework until your healthcare provider says it's OK. Talk with him or her about when it's OK to go back to work.
Do exercises as directed to help prevent swelling, keep your arm and shoulder joints flexible, and improve circulation. For instance, you may be told to squeeze a rubber ball with your hand. You may also need physical therapy after reconstruction. This is to strengthen the muscles affected by the surgery.
Wearing a breast prosthesis
A breast form (prosthesis) is a soft, breast-shaped form that fits into a bra. You may decide to use a breast prosthesis if reconstruction isn’t done at the same time as the mastectomy. Or you may use one if you choose not to have reconstruction. Some women wear breast forms to help balance weight and not have back strain. Other women wear them because they like the way they look. Talk with your healthcare provider if you want a prescription for a prosthesis.
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
Extreme chest pain or trouble breathing (call 911or other emergency service)
A fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
Chills
Pain, redness, swelling, bleeding, or drainage at the incision site
A change in the way the drainage looks or increased drainage
Cough or shortness of breath
Lower leg pain
Pain that’s not managed by medicine or gets worse
Bleeding that soaks through the bandage
Any other problems your healthcare provider told you to watch for and report
Know how to reach your healthcare provider any time problems come up. This includes after office hours, on weekends, and on holidays.
Follow-up care
You will have follow-up appointments with your healthcare provider. If you have stitches (sutures) that need to be removed, this may be done 7 to 10 days after surgery. Drains may be removed within 2 weeks. You may need to schedule more surgery for nipple and areola reconstruction. Or you may need surgery to match the remaining breast to the reconstructed one (if only one breast was affected). If you have any questions or concerns about your recovery, let your healthcare provider know.
Your long-term recovery
To help you cope with the loss of your breast, you may want to meet with a psychologist or other healthcare provider for counseling. It may also help to talk with family members and friends. Think about joining a support group as well. You may find it easier to talk with women who are going through similar experiences as you.
Risks and possible complications
Any type of surgery has some risk. Some problems related to mastectomy with reconstruction include:
Infection
Bleeding
Fluid collection (seroma)
Pain or numbness
Long-term swelling of the arm (lymphedema)
Scarring
Hardening of the breasts, damage to breast tissue, or breakdown of the implants requiring replacement (implants only)
Problems with wound healing
Muscle weakness, lumps of fat tissue at the flap donation site, or hernias (abdominal flap reconstruction only)
Not being happy with how you look after the procedure
Risks of anesthesia (the anesthesiologist will discuss these with you)
Talk with your healthcare provider about the risks related to your surgery and what you can do to help prevent problems.
Talk with him or her about what problems to look for and when to call them. Know what number to call with questions or problems, including after office hours, on weekends, and on holidays.
Updated:
February 10, 2018
Sources:
Overview of breast reconstruction, Up To Date
Reviewed By:
Gersten, Todd, MD,Stump-Sutliff, Kim, RN, MSN, AOCNS