Knee Replacement Surgery
When your knee is badly damaged by disease or injury, an artificial knee replacement may be considered. During knee replacement surgery, your joint surfaces are replaced by prostheses. These are plastic and metal parts that are used to replace your joint surfaces.
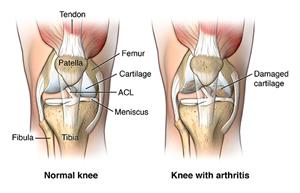
Osteoarthritis is the most common problem that leads to knee replacement surgery. This is a “wear and tear” joint disease that affects mostly middle-aged and older adults. Osteoarthritis leads to the breakdown of joint cartilage, and then bone, in your knees.
Other forms of arthritis, such as rheumatoid arthritis and arthritis caused by a knee injury, can also lead to degeneration of your knee joint. Fractures, torn cartilage, and/or torn ligaments also can lead to permanent damage to your knee joint over time.
The decision to replace the painful knee with an artificial one is a joint decision between you and your healthcare provider. Other treatments may be used first. These include lubricating injections, steroid injections, physical therapy, assistive walking devices, and anti-inflammatory medicines that help with pain and swelling.
As with most surgeries, knee replacement surgery has risks. General anesthesia is used to put you into a deep sleep during surgery. Anesthesia poses risks for some people. Other potential risks include:
- Blood clots in your legs
- Bleeding
- Infection
- Nerve or blood vessel damage
Long-term risks are not common, but can include:
- Implant problems, such as wear and loosening
- Scarring that can limit range of motion
- Continued pain
There may be other risks, depending on your specific medical condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
In addition to taking a complete medical history, your healthcare provider will do a complete physical exam. He or she may also take X-rays, urine tests, and blood tests, to check your overall health before surgery. You may also meet with a physical therapist to discuss rehabilitation after the surgery, equipment you may need (such as crutches or a walker), and modifications needed at home (for instance, toilet seat risers, tub or shower safety bars, and secure handrails at stairs).
While the chance for infection after knee replacement is very low, it can happen if bacteria enter your bloodstream. You may be asked to see your dentist before surgery, so that any major dental procedures you might need (such as tooth extractions and periodontal work) can be done before your total knee replacement surgery. This helps reduce your risk for infection.
Tell your healthcare provider about all prescription and over-the-counter medicines and any vitamins, herbs, and supplements that you are taking. Some of these may affect things like healing and blood clotting, so you may need to stop taking them before surgery.
Your healthcare provider will tell you not to eat or drink anything for several hours before the surgery. You will probably have to stay in the hospital for at least one day, and you will not be allowed to drive for some time after surgery. You will probably need some help at home (with things like bathing, dressing, cleaning, and shopping) for a short time after surgery, so you may want to arrange this ahead of time.
Talk to your healthcare provider so you know exactly what you need to do before your procedure.
Although each procedure varies, generally, surgery to replace your knee lasts about 2 hours. During surgery, you may be under general anesthesia (medicine that puts you to sleep and keeps you from feeling pain during the surgery). Your healthcare provider may also give you a nerve block, or spinal or epidural anesthesia. These numb the lower half of your body so you don’t feel pain. With these medicines, you can remain awake.
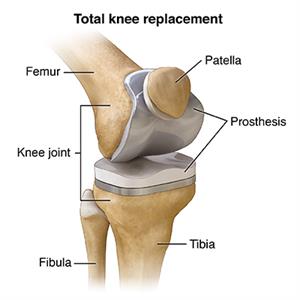
After the damaged bone and cartilage of your knee are removed, your orthopedic surgeon will put your new artificial knee in place.
The two most common types of knee prostheses used in knee replacement surgeries are cemented prosthesis and uncemented prosthesis. Sometimes, a combination of the two types is used. A knee prosthesis is made up of metal and ceramic and/or plastic. A cemented prosthesis is attached to the bone with a type of epoxy. An uncemented prosthesis attaches to the bone with a fine mesh of holes on the surface. The bone grows into the mesh and attaches naturally to the prosthesis.
The prosthesis (artificial knee) is made up of these three components:
- Tibial component (to replace the top of your tibia, or shin bone)
- Femoral component (to replace your two femoral [thighbone] condyles and the patella groove)
- Patellar component (to replace the bottom surface of the kneecap that rubs against your thighbone)
After knee replacement surgery, you will have to stay in the hospital for a day or two. While in the hospital, you will probably begin physical therapy exercises to start regaining range of motion in your knee. Physical therapy will continue at home. Pain medicines will be available to keep you comfortable. Pain management is important, because you need to start moving as soon as possible after surgery.
Your surgeon may also have you do things to help prevent blood clots and decrease swelling. For instance, you may wear special support hose, use compression boots (inflatable leg coverings) when in bed, and take blood thinners. You may also be asked to move your foot and ankle right after surgery to increase blood flow in your leg muscles and help prevent swelling and blood clots.
You may be asked to take deep breaths or use a breathing tool called a spirometer to help prevent pneumonia.
The incision (cut) will have stitches or staples that will be removed after a few weeks. Make sure you know how to care for this wound and keep it dry while it heals.
The recovery period can take anywhere from a few days to a few months. In the meantime, you may need to adjust job duties, or even take time off from work while you heal. You may need extra help at home and need to be especially careful not to fall and damage your new knee. Your healthcare provider will talk to you about activity restrictions and exercise plans you should follow after surgery.
Let your healthcare provider know about any of the following:
- Fever
- Redness, swelling, bleeding, or other drainage from the incision
- Increased pain in the knee or around the incision
These problems may need to be treated. Talk to your healthcare provider about what you should expect, and when you should see your healthcare provider right away.
Long-term outlook
- You may never get full motion in your knee, but you should be able to straighten your leg and bend well enough to climb stairs and get into a car.
- It’s normal to feel or hear clicking in your new knee.
- The incision may feel numb or stiff, especially when bending your knee.
- Your prosthesis may set off metal detectors. Tell security agents about your knee replacement.
- You will need to see your surgeon periodically for follow-up exams and X-rays, usually once a year.
- Make sure your dentist knows about your knee replacement. You will need to take antibiotics before all dental procedures for the rest of your life.
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
January 16, 2018
Sources:
Total Knee Arthroplasty. UpToDate
Reviewed By:
Ogiela, Dennis, MD,Larson, Kim APRN, FNP