Mitral valve prolapse
Mitral valve prolapse
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
American College of Cardiology/American Heart Association (ACC/AHA) Task Force, annula, annuloplasty, asymmetric mitral valve prolapse, atrial fibrillation, Calcineurin, cerebrovascular events, classic mitral valve prolapse, collagen, connective tissue disorders, dominant cutis laxa, echocardiography, Ehlers-Danlos syndrome, elastin, ErbB3, fibroblast growth factor (FGF), fibroelastic deficiency, filamin A, flail mitral valve prolapse, floppy mitral valve, Framingham Heart Study, heart attack, heart murmur, hypertrophic cardiomyopathy, infectious endocarditis, late systolic murmur, leaflet resection, leaflet thickening, left atrial enlargement, left ventricular dilatation, Marfan syndrome, mitral annulus, mitral regurgitation, mitral valve leaflets, mitral valve prolapse (MVP),MMVP1, MMVP2, myxomatous degeneration, NFAT, non-classic mitral valve prolapse, non-flail mitral valve prolapse, osteogenesis imperfecta, pseudoxanthoma elasticum, severe mitral regurgitation, Sox9, stroke, sudden cardiac death, symmetric mitral valve prolapse, three-dimensional echocardiography, transesophageal echocardiography, transforming growth factor beta (TGF-beta), two-dimensional echocardiography, Wnt/beta-catenin, X-linked valvular dystrophy.
Background
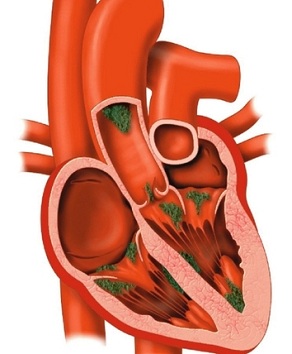
The mitral valve lies between the heart's left atrium and the left ventricle. It has two flaps (leaflets) that open and close like a pair of swinging doors. When the heart beats, the left ventricle pumps blood out to the body and the leaflets swing shut. This keeps the blood in the ventricle from going back into the left atrium. If the mitral leaflets are too floppy, big, thin, or have the wrong shape, they may not shut properly. This condition, called mitral valve prolapse (MVP), allows blood to leak back (regurgitate) into the left atrium.
MVP is a common heart valve defect. It was first described in the 1960s as a heart murmur during the late systolic (contracting) phase of the heartbeat, accompanied by prolapse (improper positioning) of one or both mitral valve leaflets. In the mid-1980s, a study using two-dimensional echocardiography suggested that MVP occurs in nearly 40% of teenage girls. However, due to increased understanding of normal heart valve structure, the definition of MVP was revised to distinguish what is true MVP vs. normal valve structure. According to the Framingham Heart Study, MVP affects between two and three percent of the U.S. population. It remains unclear how many cases are hereditary vs. idiopathic (arising suddenly from an unknown cause). Nonetheless, it is the most common cause of non-ischemic (does not stop blood flow) mitral regurgitation.
Usually, MVP is a genetic (inherited) condition that does not cause health problems. Most patients with MVP require no invasive treatment. However, rare but serious complications may occur, which include severe mitral regurgitation, infectious endocarditis (inflammation of the heart's inner lining), heart attack, stroke, or sudden cardiac death. Echocardiography, which is used to diagnose MVP, may also identify patients at high risk for complications. When necessary, treatment generally involves surgery to physically correct mitral valve defects.
Types of the Disease
True mitral valve prolapse: Mitral valve prolapse (MVP) was first described in the 1960s as a heart murmur during the late systolic (contracting) phase of the heartbeat, accompanied by prolapse (improper positioning) of one or both mitral valve leaflets. Prolapse of the mitral valve was determined by comparing its position relative to the mitral annulus, a structure that surrounds the mitral valve. MVP was diagnosed based on the assumption that a normal mitral annulus is flat (planar). It was later determined that the annulus is not planar, but rather shaped like a saddle. Because normal heart anatomy was not clearly understood until the late 1980s, many healthy individuals were initially misdiagnosed with MVP. In fact, in the mid 1980s, nearly 40% of teenage girls were diagnosed with MVP using a two-dimensional echocardiography. After normal mitral anatomy was determined using three-dimensional echocardiography, true MVP was defined as mitral leaflet prolapse of at least two millimeters in the long-axis view of the mitral valve. According to the Framingham Heart Study, MVP affects between two and three percent of the U.S. population, less than previously suggested.
Classic vs. non-classic mitral valve prolapse: Prolapse of at least five millimeters, accompanied by leaflet thickening, is defined as classic MVP. Classic MVP is associated with a higher risk of complications (such as infectious endocarditis, sudden cardiac death, heart attack, stroke, or severe mitral regurgitation).
If there is little to no thickening of the mitral leaflets, non-classic MVP is diagnosed. Non-classic MVP and prolapse of less than two millimeters are not significantly associated with the complications of classic MVP, and thus are thought to be normal variants of mitral valve structure.
Symmetric vs. asymmetric mitral valve prolapse: In classic MVP, the point where the mitral leaflets join may be even (symmetric) or uneven (asymmetric). Asymmetric MVP is more likely to result in mitral regurgitation rendering the patient more prone to deterioration of the mitral valve, and thus is more severe than symmetric MVP.
Flail vs. non-flail mitral valve prolapse: In asymmetric MVP, the structure of the mitral flaps may worsen and result in a flail leaflet, in which the tip of the mitral flap turns upward. Flail leaflets are more likely to result in mitral regurgitation, and thus are more severe than non-flail asymmetric leaflets.
Myxomatous vs. non-myxomatous mitral valve prolapse: MVP generally results from a process called myxomatous degeneration, in which the connective tissues form abnormally. This causes the mitral leaflets to enlarge and thicken. However, leaflet thickening does not occur in all cases of MVP. If the connective tissues are not sufficiently elastic (a trait called fibroelastic deficiency), the prolapsed leaflets may be thin. Another form of non-myxomatous MVP is associated with hypertrophic cardiomyopathy, in which prolapse results from elongation (but not necessarily thickening) of the mitral leaflets.
Risk Factors
Because proper connective tissue function is crucial for normal mitral valve function, connective tissue diseases may increase the risk of mitral valve prolapse (MVP). Various connective tissue disorders (including Ehlers-Danlos syndrome, osteogenesis imperfecta, dominant cutis laxa, pseudoxanthoma elasticum, X-linked valvular dystrophy, and Marfan syndrome) have been associated with MVP. About 90% of patients with Marfan syndrome also have MVP. In Ehlers-Danlos syndrome, the rate of MVP is about six percent.
Another risk factor for MVP is hypertrophic cardiomyopathy, which may cause the mitral valve leaflets to elongate or thicken. Scoliosis, some types of muscular dystrophy, polycystic kidney disease, and Graves' disease also increase the risk for MVP.
MVP occurs at equal rates in men and women. However, for reasons that are not entirely clear, men with MVP are at a higher risk of complications (such as infectious endocarditis, sudden cardiac death, heart attack, stroke, or severe mitral regurgitation) than women. One reason why MVP-related complications are generally more common in men than in women might be that severe mitral regurgitation risk increases with body weight.
Patients with classic MVP (defined as prolapse of at least 5 millimeters accompanied by leaflet thickening) also appear to be at a higher risk for complications than those with non-classic MVP (defined as prolapse with little or no mitral valve thickening). Leaflet thickening of at least 5millimeters increases the risk of complications 14-fold. Other risk factors for complications include mitral regurgitation during exercise (but not at rest).
Risk factors for cardiovascular complications (such as stroke and heart attack) include mitral regurgitation (mild to moderate) at rest, atrial fibrillation, increased age (>50 years), and enlargement of the left atrium.
Causes
Connective tissue is made of collagen and elastin, which is normally organized into fibers. In mitral valve prolapse (MVP), the fibers are often disorganized and myxomatous (gelatinous or jelly-like). This causes the mitral valve to degenerate and lose function. Myxomatous degeneration causes the mitral leaflets to enlarge and thicken. It is not entirely clear what causes myxomatous degeneration.
Non-myxomatous defects of the mitral valve (such as abnormal size or structure caused by hypertrophic cardiomyopathy) may also cause MVP.
Many proteins, tissues, and enzymes are involved in proper mitral valve development. If any of these factors are disrupted, MVP may result. Proteins that may be disrupted in MVP include calcineurin, NFAT family proteins, transforming growth factor beta (TGF-beta) proteins, fibroblast growth factors (FGFs), and Wnt/beta-catenin proteins. These proteins all producesignals that direct heart development.
Genes that may be disrupted in MVP include Sox9 and ErbB3, which are activated in the developing heart. Inherited forms of myxomatous MVP have been associated with the MMVP1 gene (linked to chromosome 16) and the MMVP2gene (linked to chromosome 11 in some families and chromosome 13 in others). It is not clear what these genes direct. However, they do not appear to be involved in producing connective tissue. This demonstrates the complex nature of mitral valve development, which involves not only genes that direct connective tissue development but also many other proteins.
Another inherited condition that may cause MVP, X-linked valvular dystrophy, involves filamin A genes on the X chromosome. These genes direct the production of connective tissue.
Signs and Symptoms
Most individuals with mitral valve prolapse (MVP) have no symptoms, and do not require treatment or close monitoring. MVP is often not diagnosed until after complications (such as infectious endocarditis, sudden cardiac death, heart attack, stroke, or severe mitral regurgitation) arise. Echocardiography may be used to identify patients at higher risk of complications.
In some patients, the mitral valve leaflets make a clicking sound when they close. A doctor may hear this when listening to the heart with a stethoscope. Individuals with MVP may also have a heart murmur, which is the sound caused by the leaking blood.
Individuals with MVP may also experience dizziness or light-headedness, anxiety, exhaustion, breathlessness (especially when playing or exercising), heart palpitations, chest pain, or fainting episodes. Symptoms of MVP in children may go away as they age.
Diagnosis
Because mitral valve prolapse (MVP) often presents with no symptoms, diagnosis is usually made during echocardiography performed for other purposes. MVP may also be diagnosed based on heart sounds in routine physical examinations, and confirmed with echocardiography. MVP is often not diagnosed until after complications arise, such as infectious endocarditis, sudden cardiac death, heart attack, stroke, or severe mitral regurgitation. Echocardiography is a non-invasive test that may also be used to diagnose and assess MVP.
MVP is most accurately diagnosed using three-dimensional echocardiography. True MVP is diagnosed if mitral leaflet prolapse is at least 2 millimeters in the long-axis view of the mitral valve. Prolapse of at least 5 millimeters, accompanied by leaflet thickening, is defined as classic MVP. If there is little to no thickening of the mitral leaflets, non-classic MVP is diagnosed. Because non-classic MVP and prolapse of less than 2 millimeters are not significantly associated with the complications of classic MVP, they are thought to be normal variants of mitral valve structure.
Transesophageal echocardiography is often used to determine the location of the prolapse (anterior, posterior, or which leaflet is prolapsed) and the severity of the prolapse (symmetric vs. asymmetric or flail vs. non-flail).
Complications
Mitral valve prolapse (MVP) is most often an inherited disorder with no symptoms. However, in rare cases, serious complications may occur. Complications associated with MVP include infectious endocarditis, sudden cardiac death, heart attack, stroke, or severe mitral regurgitation. in a subset of patients with MVP
Patients with classic MVP (defined as prolapse of at least 5 millimeters accompanied by leaflet thickening) are at a higher risk for complications than those with non-classic MVP (defined as prolapse with little or no mitral valve thickening). Leaflet thickening of at least 5 millimeters increases the risk of complications 14-fold. Other risk factors for complications include mitral regurgitation during exercise (but not at rest).
The rate of complications may be predicted by a patient's symptoms and the number of major and minor risk factors. Major risk factors include mitral regurgitation (mild to moderate) and left ventricular ejection fraction of less than 50%. Minor risk factors include mild mitral regurgitation, floppy leaflets, atrial fibrillation, increased age (>50 years), and enlargement of the left atrium. In MVP patients with no symptoms and only minor risk factors, the 10-year risk of complications is very low (2-15% for 0-2 risk factors). For MVP patients with major risk factors, the rate of complications is much higher (78% for one or more major risk factors).
Infective endocarditis: MVP increases the risk of infective endocarditis, a microbial infection of the heart, by about 800%. However, the annual risk of developing infective endocarditis in MVP patients is low (about 0.02). In MVP patients with a systolic murmur, the risk is higher (about 0.05%). Prophylactic (preventive) antibiotics may be used in high-risk MVP patients, especially those undergoing dental procedures (which increase the risk of developing infective endocarditis), those over age 50, and those with left ventricular dilatation, left atrial enlargement, or leaflet thickening.
Sudden cardiac death: Sudden cardiac death (SCD) is a rare complication of MVP, occurring in about one of every 250 cases of MVP annually (about twice the rate of the normal population). It is unclear what causes SCD in MVP patients, though arrhythmias, particularly ventricular tachyarrhythmias (abnormal heart rhythms that are rapid, with or without other abnormalities) appear to increase the risk of SCD in MVP.
Cerebrovascular ischemic events: Patients with MVP also have a 0.7% risk of cerebrovascular ischemic events, such as heart attack and stroke, which represents a slight increase (about 2-fold) over the rest of the population. The increased risk of cerebrovascular events may be caused by increased coagulation associated with mitral regurgitation.
Severe mitral regurgitation: Mitral regurgitation may progressively worsen in MVP patients, requiring corrective surgery. Severe mitral regurgitation risk increases with body weight, which may explain why MVP-related complications are generally more common in men than in women.
Treatment
Most individuals with mitral valve prolapse (MVP) have no symptoms, and do not require treatment or close monitoring. However, for symptomatic MVP, surgical repair is the treatment of choice. Experienced surgeons may also perform valve repair surgery for asymptomatic MVP if there is increased risk of complications (such as a flail asymmetric leaflet).
Surgical procedures in mitral valve repair include leaflet resection (removal). Annuloplasty (plastic repair of the heart valve) rings (rigid or flexible) may be inserted to repair the structure of the annula.
Mitral valve repair has a 10-year success rate of 93% and a 20-year success rate of 80%. Risks from the surgery include bleeding, infection, and anesthesia-associated complications. Less than one percent of patients undergoing mitral valve repair die during surgery.
Guidelines for managing patients with heart valve diseases, including MVP, are set forth by the American College of Cardiology/American Heart Association (ACC/AHA) Task Force. Interventions are categorized as ACC/AHA Classes I-III based on evidence or consensus opinion on effectiveness.
ACC/AHA Class I: For Class I recommendations, there is either evidence or consensus opinion that the interventions are useful and effective. Valve surgery is recommended for severe or acute mitral regurgitation when the valve is repairable, in symptomatic mitral regurgitation with normal left ventricular (LV) function and dimensions, and in mild-to-moderate LV abnormalities, such as enlargement, or in reduced systolic function.
ACC/AHA Class II: In Class II recommendations, there is either conflicting evidence or a disagreement about the usefulness or efficacy of an intervention.
Class IIa recommendations have evidence or opinion in favor of the intervention. Therapies in this class include surgery for severe mitral regurgitation accompanied by atrial fibrillation or pulmonary hypertension, in asymptomatic patients with atrial fibrillation and normal LV, and in patients with pulmonary hypertension.
In Class IIb recommendations, the usefulness or effectiveness of the intervention is less established by evidence or opinion. These include surgery for MVP patients in whom repair is possible, and those with refractory ventricular arrhythmias.
ACC/AHA Class III: Class III recommendations have evidence and/or consensus opinion that an intervention is not beneficial, and may, in fact, be harmful. Treatments in this class include surgery for patients in whom repair is unlikely and patients with normal LV function and no symptoms. For these patients, close monitoring is recommended instead of surgery.
Integrative Therapies
Unclear or conflicting scientific evidence:
Coenzyme Q10: Coenzyme Q10 (CoQ10) is produced by the human body and is necessary for the basic functioning of cells. Promising preliminary evidence suggests that CoQ10 supplements may help reduce the risk of cardiovascular disease, including heart attack and high blood pressure. There is also early data to support the use of CoQ10 in children with mitral valve prolapse. Well-designed clinical trials are needed before a recommendation can be made.
Magnesium: Magnesium supplementation has been reported to improve most mitral valve prolapse (MVP) symptoms. Several studies indicate patients with MVP are low in magnesium. Additional study is needed to reach a conclusion.
Historical or theoretical uses that lack sufficient evidence:
Pycnogenol: Pycnogenol® is the registered trade name for a patented water extract of the bark of the French maritime pine (Pinus pinaster ssp. atlantica), which grows in coastal southwestern France. Pycnogenol® contains oligomeric proanthocyanidins (OPCs), as well as several other bioflavonoids: catechin, epicatechin, phenolic acids (such as ferulic acid and caffeic acid), and taxifolin. Procyanidins are oligomeric catechins found at high concentrations in red wine, grapes, cocoa, cranberries, and apples. Procyanidins are often incorporated into supplements, such as Pycnogenol®, for their antioxidative properties. Pycnogenol® is thought to be beneficial for MVP, but there is a lack of research on its effectiveness.
Prevention
Mitral valve prolapse (MVP) is most often an inherited disorder with no symptoms. Therefore, prevention is not usually a consideration. However, because there is an increased risk of serious complications (such as infectious endocarditis, sudden cardiac death, heart attack, stroke, or severe mitral regurgitation) in a subset of patients with MVP, echocardiography may be used to identify patients at higher risk of complications. The appropriate treatment and preventative measures for these complications (including mitral valve surgery) then may be performed.
Prophylactic (preventative) antibiotics may be used in high-risk MVP patients, especially those with systolic murmur or those undergoing dental procedures that increase the risk of developing infective endocarditis.
Risk of cardiovascular events (such as sudden cardiac death, heart failure, heart attack, and stroke) and associated mortality may be reduced through weight loss (through diet and exercise), reducing alcohol and sodium consumption, and quitting smoking.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Akins CW, Hilgenberg AD, Buckley MJ, et al. Mitral valve reconstruction versus replacement for degenerative or ischemic mitral regurgitation. Ann Thorac Surg. 1994 Sep;58(3):668-75; discussion 675-6. View Abstract
American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006 Aug 1;114(5):e84-231. View Abstract
American Heart Association (AHA). www.americanheart.org.
Barlow JB, Bosman CK. Aneurysmal protrusion of the posterior leaflet of the mitral valve. An auscultatory-electrocardiographic syndrome. Am Heart J. 1966 Feb;71(2):166-78. View Abstract
Centers for Disease Control and Prevention (CDC). www.cdc.gov.
Criley JM, Lewis KB, Humphries JO, et al. Prolapse of the mitral valve: clinical and cine-angiocardiographic findings. Br Heart J. 1966 Jul;28(4):488-96. View Abstract
Enriquez-Sarano M, Schaff HV, Orszulak TA, et al. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation. 1995 Feb 15;91(4):1022-8. View Abstract
Framingham Heart Study. www.framinghamheartstudy.org.
Freed LA, Levy D, Levine RA, et al. Mitral valve prolapse and atrial septal aneurysm: an evaluation in the Framingham Heart Study. Am J Cardiol. 2002 Jun 1;89(11):1326-9. View Abstract
Freed LA, Levy D, Levine RA, et al. Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med. 1999 Jul 1;341(1):1-7. View Abstract
Hayek E, Gring CN, Griffin BP. Mitral valve prolapse. Lancet. 2005 Feb 5-11;365(9458):507-18. View Abstract
Levine RA, Slaugenhaupt SA. Molecular genetics of mitral valve prolapse. Curr Opin Cardiol. 2007 May;22(3):171-5. View Abstract
Levine RA, Stathogiannis E, Newell JB, et al. Reconsideration of echocardiographic standards for mitral valve prolapse: lack of association between leaflet displacement isolated to the apical four chamber view and independent echocardiographic evidence of abnormality. J Am Coll Cardiol. 1988 May;11(5):1010-9. View Abstract
Marks AR, Choong CY, Sanfilippo AJ, et al. Identification of high-risk and low-risk subgroups of patients with mitral-valve prolapse. N Engl J Med. 1989 Apr 20;320(16):1031-6. View Abstract
National Heart, Lung, and Blood Institute (NHLBI). www.nhlbi.nih.gov.
National Institutes of Health (NIH). www.nih.gov.
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Warth DC, King ME, Cohen JM, et al. Prevalence of mitral valve prolapse in normal children. J Am Coll Cardiol. 1985 May;5(5):1173-7. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017