When Your Child Has Cold Sores
When Your Child Has Cold Sores
What causes cold sores?
Cold sores are caused by the herpes simplex virus (HSV). There are 2 types of this virus. The type that usually affects the mouth is called HSV1. It’s very common in children.
HSV stays in the body once your child has it. Cold sores can appear randomly or when something triggers them. Triggers can include:
An injury to the mouth
Fever or illness
Stress
Sun exposure
Lack of sleep
Friction or rubbing mouth
What are the symptoms of cold sores?
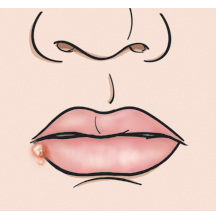
Symptoms can include tingling, burning, or itching felt in the affected area a few days before the appearance of sores. The sores themselves can cause burning, stinging, or itching. The sores are often blister-like and red at first. They then dry out and scab over. Cold sores may last 10 to 14 days.
How are cold sores spread?
Cold sores can be spread in the following ways:
Direct contact with the sores (like through touching or kissing)
Contact with items (like cups, toothbrushes, or towels) that have been contaminated by an infected person
How are cold sores diagnosed?
Cold sores are diagnosed by how they look. To get more information, the health care provider will ask about your child’s symptoms and health history. The health care provider will also examine your child. You will be told if any tests are needed. A skin biopsy or viral culture can also be performed.
How are cold sores treated?
Cold sores generally go away within 10 to 14 days with no treatment.
If your child has a sensation that a cold sore may be coming on, applying an ice cube or pack for 20 minutes may prevent it.
Ask the health care provider if there are any prescriptions or over-the-counter (OTC) medicines that will help your child feel better, faster. Topical or oral antiviral medicine can be prescribed if your child has recurrent cold sores. To be effective, the medicine needs to be taken as soon as symptoms appear.
You can do the following at home to relieve cold sore symptoms:
Make sure your child gets plenty of rest.
Give your child OTC medicines, like ibuprofen or acetaminophen, to treat pain and fever. Do not give ibuprofen to an infant less than 6 months of age, or to a child who is dehydrated or constantly vomiting. Do not give aspirin to a child with a fever. This can put your child at risk of a serious illness called Reye syndrome.
Cold liquids, ice, or frozen juice bars may help soothe mouth pain. Avoid giving your child spicy or acidic foods.
Use the following treatments only if your child is over the age of 4:
Apply an OTC numbing gel to mouth sores to relieve pain. The gel can cause a brief sting when applied.
Have your child rinse his or her mouth with saltwater or with baking soda and warm water, then spit. The mouth rinse should not be swallowed.
When to call the healthcare provider
Contact the healthcare provider if your child has any of the following:
A cold sore that doesn’t go away within 14 days
Cold sores that come back frequently
A cold sore that grows larger or appears near the eyes
Increased mouth pain
Trouble swallowing
Signs of infection around a cold sore (pus, drainage, or swelling)
Signs of dehydration (very dark or little urine, excessive thirst, dry mouth, dizziness)
Your child has a fever (see fever section below)
Your baby is fussy or cries and cannot be soothed.
Your child has had a seizure caused by the fever
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer.
For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
Ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead (temporal artery) temperature of 100.4°F (38°C) or higher, or as directed by the provider
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the provider
Child age 3 to 36 months:
Rectal, forehead, or ear temperature of 102°F (38.9°C) or higher, or as directed by the provider
Armpit (axillary) temperature of 101°F (38.3°C) or higher, or as directed by the provider
Child of any age:
Repeated temperature of 104°F (40°C) or higher, or as directed by the provider
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
How is the spread of cold sores prevented?
Follow these steps to keep your child from passing cold sores on to others:
Teach your child to wash his or her hands with soap and warm water often. Handwashing is especially important before eating or handling food, after using the bathroom, and after touching the sores.
Do not allow your child to share cups, utensils, napkins, or personal items, like towels and toothbrushes with others.
Keep your child from kissing others when he or she has a cold sore.
Keep your child’s hands out of his or her mouth. Encourage your child to not touch his or her face with his or her hands.
Wash any toys or items that your child places in his or her mouth.
Use lip balm with sun protection
Updated:
March 21, 2017
Sources:
Clinical manifestations and diagnosis of herpes simplex virus type 1 infection. UpToDate.
Reviewed By:
Dozier, Tennille, RN, BSN, RDMS,Image reviewed by StayWell medical illustration team.,Lehrer, Michael Stephen, MD