Wolff-Parkinson-White Syndrome
Wolff-Parkinson-White Syndrome
What is Wolff-Parkinson-White syndrome?
Wolff-Parkinson-White syndrome (WPW) is a type of heart condition you are born with (congenital). It causes a rapid heart rate. If you have WPW, you may have episodes of palpitations or rapid heartbeats. WPW affects between 1 and 3 of every 1,000 people worldwide.
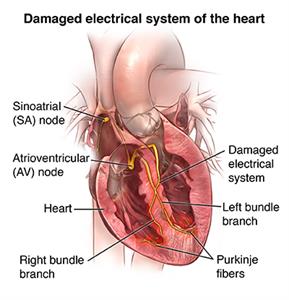
Normally, electrical signals travel through your heart in an organized way to control your heartbeat. This allows blood to pass from the upper chambers of your heart (the atria) to the lower chambers (the ventricles), and then travel out to your body. The upper and lower heart chambers are normally connected by a single main circuit in the center of the heart through which electricity flows. In WPW, there is an extra connection between the upper and lower chambers that causes a rapid heart rate (tachycardia).
What causes Wolff-Parkinson-White syndrome?
In WPW, the heart has an extra electrical pathway that causes a rapid heartbeat (tachycardia). If forms before birth as the heart is developing. It is unclear why the extra electrical pathway forms. It sometimes occurs with other congenital heart defects. A few people with WPW have a gene defect that it passed down through the family.
Who is at risk for Wolff-Parkinson-White syndrome?
WPW affects both men and women. In most cases, the cause of WPW isn’t known, but researchers have identified gene mutations that may be responsible for the disorder in a few people.
What are the symptoms of Wolff-Parkinson-White syndrome?
With WPW, you may not have any episodes of tachycardia for many years. Symptoms may also start and stop suddenly and occur at any age. Typical symptoms include:
- Shortness of breath
- A pounding in your chest
- Dizziness
- Passing out
- Cardiac arrest (rare)
How is Wolff-Parkinson-White syndrome diagnosed?
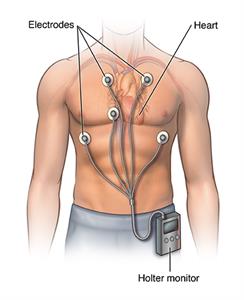
If you have symptoms of tachycardia that come and go, your healthcare provider will do a test called an electrocardiogram, or ECG. This measures the electrical activity in your heart and your heart rate. If you are not having symptoms at the time of your ECG, results may look normal. Other tests may include:
- Conducting an ECG as you walk on a treadmill (stress test)
- Wearing a type of recorder, called a Holter monitor, that takes an ECG over 24 hours
- Wearing a type of recorder, called an event recorder, that samples your heart rate over several days
- Electrophysiologic testing, a hospital procedure that involves threading catheters into your heart through a vein in your thigh
How is Wolff-Parkinson-White syndrome treated?
You may not need any treatment if you do not have symptoms, or if you have infrequent symptoms. Also, symptoms sometimes go away as people get older. If you do need treatment, there are a number of options:
- You may be able to stop an episode of tachycardia by massaging your neck, coughing, or bearing down like you are having a bowel movement. This is called a Valsalva maneuver.
- You may be able to take medicine to stop or prevent tachycardia. But, there is no medicine that will cure this condition.
- If medicine and the Valsalva maneuver do not work, you may need to go to the hospital for cardioversion. This procedure restores your heartbeat to a normal rhythm, by passing an electric current through your chest into your heart.
- If you are having frequent or uncontrolled episodes of tachycardia, you may have a procedure called radiofrequency ablation. Your doctor threads a long, thin, flexible tube (catheter) through a vein in your groin to the heart. There, low-voltage, high-frequency electrical energy is used to destroy the abnormal connection. The treatment cures WPW about 95% of the time.
What are the complications of Wolff-Parkinson-White syndrome?
WPW is not a dangerous disease for most people. You can manage or correct the condition with treatment. Worrisome symptoms include fainting with very rapid heart rates. There is a very small risk of cardiac arrest if the heart rate becomes extremely rapid. This may be seen in people who also have atrial fibrillation (another type of arrhythmia).
How can I manage Wolff-Parkinson-White syndrome?
There is no way to prevent WPW, but you can prevent complications by learning as much as you can about the disease. Work closely with your cardiologist (healthcare provider who specializes in diseases of the heart) to find the best treatment. Ask him or her to teach you how to do a Valsalva maneuver.
Here are helpful lifestyle suggestions:
Don't smoke.
Work with your healthcare provider to keep conditions like high cholesterol and high blood pressure under control.
Eat a heart-healthy diet.
Maintain a healthy weight.
Get regular exercise.
Tell your healthcare provider right away if you have symptoms of WPW.
Key points
- Wolff-Parkinson-White syndrome is a type of heart defect that you are born with. It causes rapid heart rate.
- Medicine can help control symptoms.
- Cardiac ablation can cure the disease in many cases.
- Consult with your healthcare provider right away if you have symptoms of Wolff-Parkinson-White syndrome.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
April 09, 2017
Sources:
WPW- Beyond the Basics, Up To Date, Treatment of symptomatic arrhythmias associated with Wolff-Parkinson-White Syndrome, Up To Date
Reviewed By:
Fetterman, Anne, RN, BSN,Kang, Steven, MD