Understanding Hydrodistention with Cystoscopy
Understanding Hydrodistention with Cystoscopy
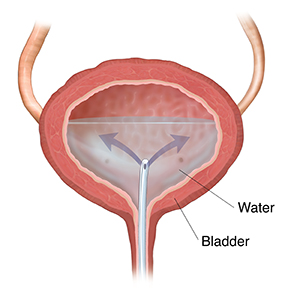
Hydrodistention is a procedure that fills up your bladder with water. It is used to help find out what may be causing your bladder pain. During the procedure a long, thin tube (cystoscope) is used. It has a lens and a light on one end. This tube helps your healthcare provider see inside your bladder. It is put into your bladder through your urethra. That’s the tube that passes urine out of your body.
How to say it
hy-droh-dis-TEN-shun sis-TOHS-kuh-pee
Why hydrodistention with cystoscopy is done
This procedure is often done to figure out the cause of bladder pain. It may help diagnose bladder pain syndrome (BPS), also called interstitial cystitis (IC). If you have this health problem, you may feel pain when your bladder fills with urine. You may also need to pass urine more often.
This procedure is also sometimes done to treat BPS. It may be tried if other treatments, such as medicine, don’t work.
How hydrodistention with cystoscopy is done
This may be done in a hospital or at an outpatient facility. During the procedure:
-
You are given medicine so you won’t feel any pain. It may also make you fall asleep.
-
Your healthcare provider puts the cystoscope into your urethra. He or she gently moves it forward into your bladder.
-
Using the cystoscope, he or she slowly fills up your bladder with as much water as possible. This helps find out how much fluid your bladder can hold.
-
Your bladder is then drained and filled again.
-
Your healthcare provider may look at your bladder lining with the cystoscope. He or she will see if there are any sores or other possible causes for your symptoms.
-
Your bladder is drained.
Risks of hydrodistention with cystoscopy
All procedures have risks. Some possible risks of this procedure include:
-
Infection
- Blood in urine
-
Symptoms get worse
Updated:
September 17, 2019
Sources:
Clemens JQ. Management of interstitial cystitis/bladder pain syndrome. Up To Date. July 23 ed: Up To Date; 2015. p. 16., Clemens JQ. Pathogenesis, clinical features, and diagnosis of interstitial cystitis/bladder pain syndrome. Up To Date. July 24 ed: Up To Date; 2015. p. 17., Clemens JQ. Treatment of interstitial cystitis/bladder pain syndrome (Beyond the Basics). Up To Date. July 24 ed: Up To Date; 2015. p. 8., Ferri F. Interstitial Cystitis In: Ferri F, editor. Ferri's Clinical Advisor 2016. Philadelphia: Elsevier; 2016. p. 712-3., Hanno PM, et al. Diagnosis and Treatment of Interstitial Cystitis/Bladder Pain Syndrome. American Urological Association (AUA) Guideline. 2014:45., Meijlink JM, et al. Interstitial Cystitis, Bladder Pain Syndrome, Painful Bladder Syndrome, Hypersensitive Bladder, Chronic Pelvic Pain, Associated Disorders. Rotterdam: International Painful Bladder Foundation (IPBF); 2014.
Reviewed By:
Marc Greenstein MD,Donna Freeborn PhD CNM FNP,Raymond Kent Turley BSN MSN RN