Understanding Coccydynia
Understanding Coccydynia
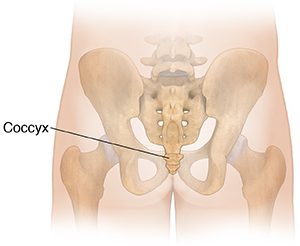
Coccydynia is pain at the lowest tip of the spine (the coccyx, or tailbone). This is sometimes called a “bruised tailbone.” Tailbone pain can be very uncomfortable. It can also interfere with daily activities, such as driving.
How to say it
kok si DIN ee uh
What causes coccydynia?
Causes of tailbone pain include:
-
Injury to the tailbone from a blow or fall
-
A bone spur on the tailbone
-
Poor posture while sitting
-
Sitting for a long time in an uncomfortable position
-
Vaginal childbirth
-
Arthritis
In some cases, the cause of the pain can’t be found.
Symptoms of coccydynia
You may feel:
-
A dull ache or sharp pain in the tailbone area, near the top of the buttocks
-
Muscle spasms in the lower back or pelvic area
-
A sense of pressure in the rectum
Pain may be triggered by things like walking or standing up from sitting. It may hurt more if you sit for long periods. Things that put pressure on the tailbone, such as riding a horse or having sex, may also trigger the pain.
Treatment for coccydynia
Tailbone pain often goes away by itself within a few months. Treatment focuses on reducing pain and protecting the tailbone. Treatments can include:
-
Over-the-counter or prescription medicine to help relieve pain and swelling. NSAIDs (nonsteroidal anti-inflammatory drugs) are the most common medicines used. Medicines may be prescribed or bought over the counter. They may be given as pills. Or they may be put on the skin as a gel, cream, or patch.
-
Warm or cold to help relieve symptoms for a time, such as a heating pad, hot water bottle, or ice pack
-
Keeping pressure off the tailbone to help the area heal by shifting weight forward onto your hipbones and thighs when sitting or sitting on a special cushion
-
Medicine injected into the area to help relieve severe symptoms. The medicine is usually a corticosteroid. This is a strong anti-inflammatory medicine.
-
Physical therapy to help strengthen the structures around the tailbone
If no other treatments work, you may need surgery to remove all or part of the coccyx.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Pain that continues for more than 2 months or gets worse
-
Pain that limits your usual activities
-
Pain that doesn’t get better by trying the self-care treatments described above
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider
- Chills
-
Redness or swelling
-
A new sore in the cleft of the buttocks, especially one that contains or drains pus
-
Other new symptoms
Updated:
September 17, 2019
Sources:
Buttaravoli P, Leffler SM. Coccyx Fracture. In: Buttaravoli P, Leffler SM, editors. Minor Emergencies. 3 ed. Philadelphia: Saunders; 2012. p. 410-1., Choi SB, et al. Pelvic Trauma. In: Marx JA, et al, editors. Rosen's Emergency Medicine. 8 ed. Philadelphia: Saunders; 2014. p. 656-71., Foye PM. Coccydynia (coccygodynia). UpToDate. December 14 ed: UpToDate; 2015. p. 14., Maigne JY. Coccydynia. In: Slipman CW, et al, editors. Interventional Spine: An Algorithmic Approach. Philadelphia: Elsevier; 2008. p. 1289-97., Vora A, Yin AX. Coccydynia. In: Frontera WR, et al, editors. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. 3 ed. Philadelphia: Saudners; 2015. p. 490-4., Waldman SD. Coccydynia. In: Waldman SD, editor. Pain Management. 2 ed. Philadelphia: Saunders; 2011. p. 801-3.
Reviewed By:
Raymond Kent Turley BSN MSN RN ,Kenny Turley PA-C,L Renee Watson MSN RN