Treatment for Your Child’s Atrial Septal Defect (ASD)
Treatment for Your Child’s Atrial Septal Defect (ASD)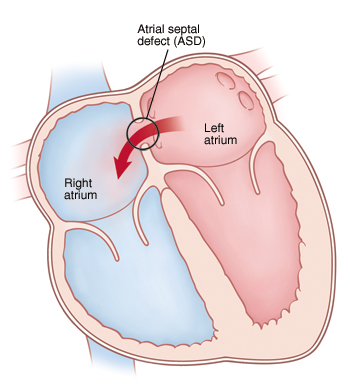
Your child has an atrial septal defect (ASD). This is a hole in the dividing wall (atrial septum) between the 2 upper chambers (atria) of the heart. Your child’s cardiologist has determined that the ASD won’t close on its own and has suggested repair. ASD repair can be done either with cardiac catheterization or with open heart surgery. Your child’s cardiologist or surgeon will discuss the best treatment for your child with you. Typically, only isolated secundum type ASDs (ASDs present in the center portion of the atrial septum) can be closed via cardiac catheterization. All other types of ASDs require open heart surgery.
Your child’s experience: cardiac catheterization
Cardiac catheterization is a procedure done on the heart using a thin, flexible tube called a catheter. It’s done by a cardiologist who has special training to use catheters to treat heart problems (cardiac catheterization). The procedure lasts about 2 to 4 hours. It takes place in a catheterization lab. You’ll stay in the waiting room during the procedure:
Before the procedure
You’ll be told to keep your child from eating or drinking anything for a certain amount of time before the procedure. Follow these instructions carefully.
During the procedure
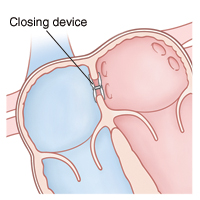
Your child is given medicine (sedative or anesthesia). This is to help him or her relax and not feel discomfort or pain during the procedure. A breathing tube may be put in your child’s windpipe (trachea). Special equipment monitors your child’s heart rate, blood pressure, and oxygen levels. The catheter insertion site (the groin) is cleaned and numbed. Then the catheter is put into a blood vessel in the groin. With the help of live X-rays, the catheter is moved up through this blood vessel into the heart. Contrast dye may be injected through the catheter. The dye allows the doctor to see the inside of the heart more clearly on X-rays. A closure device is used to close the ASD. It’s delivered by the catheter and placed across the ASD. Then the catheter is removed.
After the procedure
Your child is taken to a recovery room. You can stay with your child during much of this time. It may take 1 to 4 hours for medicines to wear off. Pressure is put on the catheter insertion site to limit bleeding. The doctor or nurse will tell you how long your child needs to lie down and keep the insertion site still. Your child is cared for and monitored until he or she can leave the hospital. Your child will usually need to stay overnight in the hospital.
Risks and possible complications of cardiac catheterization
Reaction to contrast dye
Reaction to sedative or anesthesia
Pain, swelling, redness, bleeding, or drainage at the catheter insertion site
Wound infection at catheter insertion site
Incomplete closure of the ASD, needing more treatment
Abnormal heart rhythm (arrhythmia)
Injury to the heart or a blood vessel
Unexpected movement of the device (device embolization). This is rare, but means the device needs to be removed right away.
Your child’s experience: heart surgery
Heart surgery to repair an ASD is done by a pediatric heart surgeon. The surgery lasts about 2 to 3 hours. It takes place in an operating room in a hospital. You’ll stay in the waiting room during your child’s surgery.
Before surgery
You’ll be told to keep your child from eating or drinking anything for a certain amount of time before surgery. Follow these instructions carefully.
During surgery
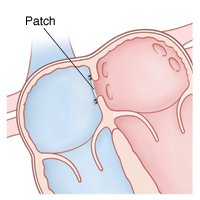
Your child is given medicine (sedative and anesthesia) to sleep and not feel pain during surgery. A breathing tube is put in your child’s windpipe (trachea). Special equipment monitors your child’s heart rate, blood pressure, and oxygen levels. Your child is also placed on a heart-lung bypass machine. This allows blood to continue flowing to the body while the heart is stopped so that it can be operated on. The surgeon makes an incision in the chest through the breastbone (sternum) to reach the heart. The ASD is repaired with either stitches or a patch. Then your child is taken off the bypass machine and the chest is closed.
After surgery
Your child is taken to a critical care unit to be cared for and monitored. You can stay with your child during much of this time. He or she may remain in the hospital for 3 to 5 days. When your child is ready to leave the hospital, you’ll be given instructions for home care and follow-up. Your child's cardiologist may recommend that your child take antibiotics before having dental work. The cardiologist will tell you how long this should continue.
Risks and possible complications of heart surgery
Reaction to sedative or anesthesia
Incomplete closure of the ASD, requiring further treatment
Abnormal heart rhythm (arrhythmia)
Wound infection
Infection
Bleeding
Nervous system problems, such as seizures or stroke
Abnormal buildup of fluid around the heart and lungs
When to call the doctor
After the cardiac catheterization procedure or heart surgery, call the doctor right away if your child has:
Increased pain, swelling, redness, bleeding, or drainage of an incision or insertion site
A fever. Talk with your child's doctor to find out at what temperature you should be concerned.
Chest pain
Increased tiredness
Trouble breathing
Nausea or vomiting that continues
A cough that won’t go away
An irregular heartbeat
Passing out
Updated:
August 16, 2018
Sources:
Management and outcome of isolated atrial septal defects in children, Up To Date
Reviewed By:
Ayden, Scott, MD,Bass, Pat F. III, MD, MPH,Image reviewed by StayWell medical illustration team.