Overactive Bladder Syndrome (OAB)
Overactive Bladder Syndrome (OAB)
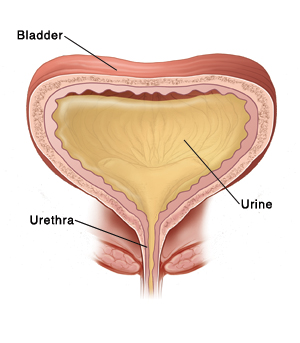
When the bladder muscle contract or squeeze involuntarily, it is called overactive bladder syndrome. This causes an intense urge to urinate, known as urgency. Urgency can occur many times during the day and night. If urine leaks with the urgency, it is called urge incontinence.
A disease that affects the bladder nerves, such as multiple sclerosis, can cause overactive bladder syndrome. Other conditions, such as urinary tract infection (UTI) or prostate problems in men, can also lead to OAB. But the exact cause is often not known.
How is overactive bladder syndrome diagnosed?
Your healthcare provider will examine you and ask about your symptoms and health history. You may also have one or more of the following:
Urine test to take samples of urine and have them checked for problems.
Urinary diary to record how much fluid you take in and urinate out in a 3 day period.
Bladder ultrasound to study the bladder as it empties. Ultrasound uses sound waves to create detailed images of the inside of the body.
Cystoscopy to allow the healthcare provider to look for problems in the urinary tract. The test uses a thin, flexible scope called a cystoscope with a light and camera on the end. The scope is inserted into the urethra (the tube that carries urine out of the body).
Urodynamic studies, a battery of tests designed to measure and record many aspects of urinary bladder function, including pressures, volume, and urine flow.
How is overactive bladder syndrome treated?
Treatment depends on the cause and severity of your OAB. Treatments may include the following:
Changing urination habits may be suggested. For instance, your healthcare provider may suggest that you urinate as soon as you feel the urge. You may also need to limit how much fluid you have during the day.
Exercising your pelvic muscles can help strengthen muscles used during urination. These exercises are called Kegels. They involve contracting as if you were stopping your urine stream and tightening your rectum as if trying not to pass gas. Your healthcare provider can help you learn how to do Kegels.
Biofeedback to help you learn to control the movement of your bladder muscles. Sensors are placed on your abdomen. They turn signals given off by your muscles into lines on a computer screen.
Medicine may be given to relax the bladder muscle. Medicine can also help ease bladder contractions, which reduces the urge to urinate.
Neuromodulation may be done if medicine and behavioral changes don’t work. Electrical pulses are sent to the sacral nerves (nerves that affect the pelvic area). These pulses help relieve OAB and urge incontinence.
Surgery to make the bladder larger may be done in severe cases.
With treatment, OAB can be managed. A condition, such as UTI, that has caused you to have OAB will be treated. Treatment may involve taking medicine for months or years. You may also need to make changes in your daily routine. This may include going to the bathroom more often than you think you need to. Or, you may need to cut back on caffeine and alcohol because these can make symptoms worse. Your healthcare provider can tell you more.
When to call your healthcare provider
Call the healthcare provider right away if you have any of the following:
Fever of 100.4°F (38.0 °C) or higher
No improvement with treatment
Trouble urinating because of pain
Back or abdominal pain
Updated:
March 21, 2017
Sources:
Gormley, EA. Diagnosis and Treatment of Overactive Bladder in Adults: American Urology Association/Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction Guideline. The Journal of Urology (2012); 188(6) s2455-s2463, Winters, JC, et al. Urodynamic Studies in Adults: American Urological Association/Society for Urodynamics and Female Urology. The Journal of Urology (2012); 188 (6); pp. s2464-s2472
Reviewed By:
Goode, Paula, RN, BSN, MSN,Greenstein, Marc, DO,Image reviewed by StayWell medical illustration team.