Ocular Histoplasmosis Syndrome
Ocular Histoplasmosis Syndrome
Ocular histoplasmosis syndrome (OHS) is a disease that can cause vision loss.
Understanding OHS
Experts believe that OHS is caused by a fungus called Histoplasma capsulatum. This fungus is found in the dust and soil. It is found mainly in the Mississippi and Ohio River Valleys of the U.S. If you breathe it into your lungs, the fungus can cause histoplasmosis. This is often a mild condition with flu-like symptoms. Or there may be no symptoms at all. It often goes away without treatment. But once it’s in your body, the fungus can also affect your eyes. This is called OHS.
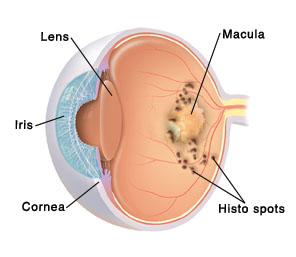
OHS causes inflammation in the choroid. The choroid is a layer of blood vessels under your retina (the light-sensing layer of tissue at the back of your eye). The inflammation leaves scars called histo spots.
As OHS gets worse, abnormal blood vessels can grow from a layer of otherwise normal blood vessels called the choroid. These blood vessels are called CNV (choroidal neovascularization). In some cases, the CNV sores (lesions) leak blood and fluid into the center part of the retina (the macula). The macula plays a key role in helping you see clearly. If CNV lesions leak into the macula, your vision can become blurry and distorted. If you have CNV in one eye, you may later get it in your other eye.
Risk factors for OHS
Only a small number of people infected with histoplasmosis will develop OHS. But you are at risk for OHS if you:
Have had histoplasmosis
Live in the Ohio or Mississippi River Valleys
Signs and symptoms of OHS
Most people with OHS never have any symptoms. As the disease gets worse, an eye healthcare provider may find histo spots during an eye exam. You may notice vision changes such as:
A blind spot in your eye
Straight lines appearing crooked or wavy
Diagnosis of OHS
An eye healthcare provider can check for OHS. You will be given special eye drops. These will enlarge (dilate) the dark circles in the center of your eyes (your pupils). Your eyes will then be checked. A test called fluorescein angiography may also be done. With this test, a special dye (fluorescein) is injected into a vein in your arm. The dye travels to the blood vessels in your choroid and your retina. The dye lets your eye healthcare provider see any histo spots and CNV.
Treatment of OHS
If your macula is not damaged, OHS does not need treatment. When the macula is affected, there are three main types of treatment:
Medicines injected into your eye. These medicines can be used for CNV that is under the very center of the macula or elsewhere. They limit abnormal blood vessel growth. First your eye is numbed. Then the medicine is injected. These injections must often be repeated, but some people can go for years without needing more treatment.
Photodynamic therapy. A medicine is injected into a vein in your arm and collects in the CNV. A laser (a special focused beam of light) is then used to treat the CNV. The laser causes the medicine to close off the abnormal blood vessels in the CNV. Like medicines injected into the eye, this treatment can be repeated, but people can go for years without needing more treatment.
Photocoagulation. With this surgery, a special laser destroys the abnormal blood vessels in the retina. This is for people whose CNV is not below the very center of the macula. That’s because the laser burns the retina along with the CNV. It causes a blind spot wherever treatment is done.
Checking for macular damage
To see if you have macular damage, your eye healthcare provider may suggest that you use an Amsler grid. This can be helpful if you have already had treatment. It can also be helpful if you have histo spots but no vision loss. An Amsler grid is a simple lined grid with a dot in the middle. You will be asked to look at it. If your macula is damaged, the grid’s lines may look curved to you. Or a blank spot may seem to appear.
Updated:
January 01, 2018
Reviewed By:
Bogus, William J, OD, FAAO,Haupert, Christopher L., MD