Necrotizing Enterocolitis (NEC) in the Newborn
Necrotizing Enterocolitis (NEC) in the Newborn
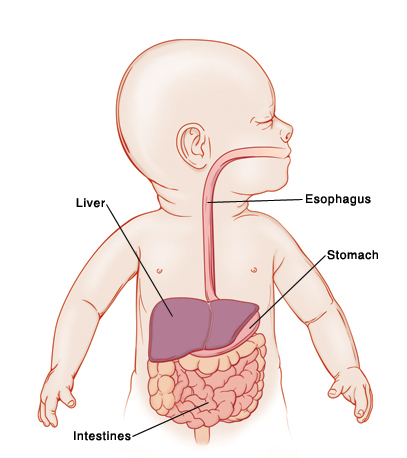
NEC is a serious medical problem. It occurs when an area of the baby’s bowel (intestine) becomes damaged. This damage happens when a portion of intestines isn’t getting enough oxygen. This causes the tissue to die (become necrotic). Bacteria in the bowel may then begin to destroy tissue from the inner layers of the bowel, spreading outward. NEC is more common in premature infants because the bowel is not yet mature.
How is NEC diagnosed?
NEC is suspected if the baby has trouble tolerating feeds, vomits, or has large residuals (food remaining in the stomach). The baby may also have blood in the stool and a bloated abdomen. An X-ray image can show thickening of the bowel wall. It may also show bubbles of gas in the bowel wall. NEC is an inflammation of the bowel that can be very serious. The exact cause of NEC is not known, but it happens more often in premature babies, especially those who have not received human milk. Human milk has many protective factors that formula can't provide, but even premature babies who haven't received formula can get NEC. The earlier the baby, the higher the risk.
What is a “NEC watch" or "NEC scare”?
Babies who are born premature or who have medical problems are treated in the NICU (neonatal intensive care unit). NICU staff may suspect that a baby’s bowel may be damaged. This may be referred to as "NEC watch" or "NEC scare" In many cases, this can be prevented from turning into NEC. Breast milk or formula feedings are stopped, and the baby is given nutrition through a tube in a vein (called total parenteral nutrition or TPN). This allows the bowel to rest. The baby will most likely be given antibiotics to prevent infection. In many cases, there is no lasting damage to the bowel, and no further treatment is needed.
How is NEC treated?
A baby with NEC will first be evaluated to see if emergency surgery is needed. Treatment may consist of:
Medical treatment. Enteral feedings (feedings through the digestive tract) are stopped to rest the bowel. The baby is fed with TPN. Antibiotics are used to prevent infection and further damage. If the baby is extremely ill, or doesn’t begin to get better within a couple of days, surgery may be the next step. In some cases, babies are treated with probiotics, which are live microorganisms that are introduced into the digestive tract.
Surgery to do any or all of the following, depending on the location and severity of the damage:
Place a drain into the abdominal cavity to relieve pressure and inflammation. This allows the bowel to rest and heal.
Remove part of the bowel. The necrotic or dead portion of the bowel is removed. This protects the remaining bowel and allows it to heal.
Place an enterostomy to let a portion of the bowel heal by rerouting the stool. In this case, the surgeon will create an enterostomy (also called an ostomy or a stoma). This is done by bringing the open ends of the bowel through an incision in the abdomen. A stoma keeps waste from traveling through the part of the bowel that needs to rest. After the bowel has healed, the ends are then reconnected, and the ostomy is closed.
What are the long-term effects?
Many babies with NEC have no lasting damage. But NEC can cause serious ongoing problems and can be life threatening. If surgery is needed, the outcome depends on how much bowel is removed. Sometimes the remaining bowel can take over the functions of the part of the bowel that was removed. In some cases, the baby can’t absorb certain nutrients and may need to be on a special diet. In other cases, the child may have a permanent stoma. But a child can thrive with a stoma, or even with much of the colon (large intestine) removed. In rare cases, so much bowel is removed that the baby needs to stay on TPN for an extended period. This can have other side effects such as infection or liver damage.
Updated:
January 20, 2018
Sources:
Clinical features and diagnosis of necrotizing enterocolitis in newborns, Up To Date, Gephard, SM, Necrotizing Enterocolitis Risk: State of the Science, Advances in Neonatal Care (2012); 12(2); 77-89, Li, D., Probiotics for the prevention of necrotizing enterocolitis in neonates: an 8-year retrospective cohort study, Journal of Clinical Pharmacy and Therapeutics (2013); 38; 445-449, Management of necrotizing enterocolitis in newborns, Up To Date, Pathology and pathogenesis of necrotizing enterocolitis in newborns, Up To Date, Prevention of necrotizing enterocolitis in newborns, Up To Date
Reviewed By:
Freeborn, Donna, PhD, CNM, FNP,Lee, Kimberly, G., MD, MSc, IBCLC