Marfan syndrome
Marfan syndrome
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Aneurysm, aortic aneurysm, aortic dissection, aortic rupture, arachnodactyly, autosomal dominant disorder, autosomal dominant trait, cataract, connective tissue, connective tissue disorder, detached retina, dural ectasia, endocarditis, fibrillin, Ghent criteria, glaucoma, heart surgery, mitral valve prolapse, retinal tears, scoliosis, spondylolisthesis, stretch marks.
Background
Marfan syndrome, also called arachnodactyly, is a genetic disorder that causes the connective tissues to become weak and dysfunctional. These tissues, which include tendons, ligaments, cartilage, and bone, are important because they support the body and provide a framework for growth and development. Because connective tissues are found throughout the body, symptoms may develop in many body organs, including the eyes, bones, heart, blood vessels, skin, lungs, and nervous system.
The severity of disease symptoms varies from mild to severe. For instance, Marfan syndrome can be life threatening if it affects the aorta, the main artery that carries blood from the heart to the rest of the body. In such cases, the disorder causes the walls of the aorta to become weak, increasing the chance that the artery will enlarge, tear, or rupture (break open). In other cases, patients may not experience any noticeable symptoms.
Physical characteristics commonly associated with Marfan syndrome include a slender and tall body, loose joints, narrow face, and spinal or chest wall abnormalities, such as scoliosis. Some medical historians believe that Abraham Lincoln may have had Marfan syndrome, because he had many of these traits. However, Lincoln's physical features alone are not enough to determine whether he had the disorder.
Researchers estimate that Marfan syndrome affects at least one out of 5,000 people in the United States.
Although Marfan syndrome is a serious and potentially life-threatening condition, patients are able to live long, healthy lives with proper treatment. There is currently no cure for the disorder. Instead, treatment focuses on managing symptoms and preventing complications. Most people with Marfan syndrome are able to have children, although complications may occur during pregnancy, and parents may pass on the condition to their children.
Risk Factors
The only known risk factor for Marfan syndrome is a family history. If one parent has Marfan syndrome, there is a 50% chance that his or her child will have Marfan syndrome. If both parents have Marfan syndrome, there is a 75% chance that their child will inherit the condition.
Causes
General: Marfan syndrome is a disorder that causes the connective tissues to become weak and dysfunctional. These tissues, which include tendons, ligaments, cartilage, and bone, are found throughout the body. They are important because they support the body and provide a framework for growth and development. In healthy individuals, the connective tissues are made up of proteins, including the structural proteins collagen and elastin and specialized proteins such as fibrillin and proteoglycans.
People with Marfan syndrome are born with a mutated, or abnormal, fibrillin gene. This gene normally produces fibrillin, a vital component of healthy connective tissues. Mutations in this gene may lead to deficient levels of fibrillin in connective tissues. As a result, the connective tissues may stretch abnormally when they are subjected to stress or physical strain.
Inheritance: Most cases of Marfan syndrome are inherited, or passed down from a parent, as an autosomal dominant trait. This means that only one copy of the defective gene must be inherited for the disease to appear. If one parent has Marfan syndrome, there is a 50% chance that his or her child will have Marfan syndrome. If both parents have Marfan syndrome, there is a 75% chance that their child will inherit the condition.
Random mutation: About 25% of patients with Marfan syndrome did not inherit the condition from their parents. Instead, the genetic mutation occurs randomly during the development of the egg cells, sperm cells, or embryo. It is theoretically possible for a person who randomly acquires this mutation to pass on the disorder to his or her children.
Signs and Symptoms
General: Because connective tissue is found throughout the body, there are many possible signs and symptoms of the disorder, which range from mild to severe. Symptoms may vary even among members of the same family. Some people may not notice symptoms or may not develop symptoms until adulthood, while others experience more serious symptoms at an early age. In most cases, symptoms worsen with age.
The heart and arteries are most commonly affected by Marfan syndrome. Symptoms affecting the heart and arteries are usually the most severe and account for most of the deaths related to the disorder. Vision and skeletal problems are also common, because the eyes and bones are made up of connective tissue. Below are some of the most common symptoms of Marfan syndrome.
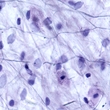
Physical characteristics: Many people with Marfan syndrome have distinct physical features. They are often slender and tall, with exceptionally long spider-like fingers and toes (called arachnodactyly). Their arms and legs are often disproportionately long in relation to their bodies. People may also have excessively flexible or loose joints, scoliosis (curvature of the spine), a narrow face, a high and arched palate, crowded teeth, flat feet, and a chest that is either concave or protrudes outward. This is because connective tissue supports the body and provides a framework for growth and development.
Aortic aneurysm: Aortic aneurysms may occur in patients with Marfan syndrome, because the connective tissues in the arteries are weaker than normal. An aortic aneurysm occurs when the large artery in the heart, called the aorta, has a bulge. Some patients may have no symptoms, while others may experience shortness of breath. Over time, the aorta may continue to bulge even more. This increases the risk of complications, such as a ruptured artery or aortic dissection.
Mitral valve prolapse: A mitral valve prolapse may also occur. This happens when the valve that separates the left and right side of the heart bulges backward into the left side of the heart, also called the left atrium. This prevents the valve from closing properly and allows blood to leak from the ventricle back into the atrium. In milder cases, a mitral valve prolapse does not cause symptoms and is not cause for concern. However, if the valve leaks a lot of blood, it may cause irregular heartbeats and increase the risk of heart infection. In severe cases, a person may have difficulty breathing.
Vision problems: Individuals with Marfan syndrome may experience several eye-related symptoms. The lens may become dislocated in one or both eyes. This can happen if the ligaments that hold the lens in place are weaker than normal. Some individuals with Marfan syndrome may experience extreme nearsightedness.
Some individuals may develop glaucoma, an increased pressure inside the eyeball that is caused by many factors. Left untreated, this increase in pressure may cause permanent damage to the optic nerve and retinal fibers, which may in turn lead to progressive and permanent loss of vision. Symptoms range from glare and light sensitivity to severe eye pain, blurred vision, and blindness.
Some patients with Marfan syndrome may develop cataracts, in which the clear lens of the eye becomes cloudy. Retinal tears or detachments may also occur. The retina, located at the back of the eye, sends visual images to the brain for interpretation. Tears often develop before the retina starts to detach from the back of the eye. Retinal detachment occurs when the retina separates from the connective tissue at the back of the eyeball.
Scoliosis: About 50% of individuals with Marfan syndrome develop scoliosis, or curvature of the spine. Only about 33% of people with Marfan syndrome and scoliosis require treatment for back problems.
Spondylolisthesis: Some people develop spondylolisthesis, a condition that occurs when one vertebra slips over another. Although spondylolisthesis does not usually cause permanent damage, it may lead to back pain and stiffness.
Foot pain: Many people with Marfan syndrome have long, slender feet that are flatter than normal. These physical features may lead to long-term foot pain.
Stretch marks: People with Marfan syndrome may develop stretch marks on their skin. This is because they lack fibrillin, which helps the skin stay firm. Stretch marks are most common on the hips, lower back, and shoulders. Stretch marks often fade over time.
Dural ectasia: The brain and spinal cord are surrounded by fluid that is enclosed in a tough membrane called the dura. In people with Marfan syndrome, the connective tissue of the dura may weaken and start to expand. This condition, which is called dural ectasia, is most common in older adults. The risk of developing this condition increases with age. Without treatment, the membrane may press on the vertebrae in the lower back. Symptoms typically range from a mild ache or soreness in the lower back to headache, abdominal pain, and pain or numbness in the legs.
Diagnosis
General: Marfan syndrome is often difficult to diagnose because the symptoms vary widely, even among members of the same family. Guidelines, known as the Ghent criteria, have been developed to help doctors diagnose the disorder.
Ghent criteria: If a person has a family history of Marfan syndrome, he or she must have one of the major criteria in one organ system and the involvement of another organ system in order to be diagnosed with the disorder. If an individual is suspected of having Marfan syndrome, but he or she does not have a family history of the disorder, two major criteria affecting different organs and the involvement of another organ are required for a diagnosis.
These criteria are as follows: (1) aortic dissection of the ascending aorta, (2) an enlarged aorta, (3) dislocation of the lens of one or both eyes, (4) dural ectasia, (5) at least four abnormalities in the bones (such as chest deformities; abnormally long arms, legs, fingers, or toes; flat-footedness; or scoliosis), (6) a family history of Marfan syndrome, and (7) having the mutated gene associated with Marfan syndrome.
Genetic testing: No currently used diagnostic test can rule out Marfan syndrome. For example, some tests may not find the genetic mutation even if it is present. Others may confuse Marfan syndrome with another connective tissue disorder. Furthermore, if the genetic mutation is detected, this test cannot predict how severe the disorder will be.
However, genetic testing may be helpful for some people. For instance, if a prospective parent has Marfan syndrome, genetic testing may be used during pregnancy to determine whether a developing fetus may have the disorder. Patients should thoroughly discuss the potential health risks and benefits of prenatal testing with their doctors or genetic counselors before making any health-related decisions.
Complications
General: In order to avoid complications, people with Marfan syndrome should visit their doctors regularly. Doctors usually check for signs of complications, especially in the heart.
Aortic dissection: Marfan syndrome causes the aortic walls to be weaker than normal. People with Marfan syndrome may therefore develop an aortic dissection or rupture. An aortic dissection occurs when a tear develops in the wall of the aorta. If the tear goes all the way through the aortic wall, it is called a rupture. A dissection or rupture may block blood flow to other arteries that branch off from the aorta. Blood may leak and accumulate in the chest, pericardial sac, or the space between the two membranes that surround the heart. An aortic dissection is a life-threatening emergency that requires immediate medical attention. Fewer than 50% of people with aortic dissections survive.
Endocarditis: People with a heart defect called a mitral valve prolapse have an increased risk of acquiring endocarditis, or heart valve infection. This happens when microorganisms, usually bacteria, enter the bloodstream, travel to the heart, and infect heart valves. Some doctors prescribe antibiotics before dental and surgical procedures to help reduce this risk.
Enlarged heart: The heart may become enlarged if a person has a severe mitral valve prolapse. This is because the heart has to work harder to pump blood throughout the body. This may lead to irregular heartbeats and congestive heart failure.
Lung problems: Because people with Marfan syndrome have connective tissue deficiencies, they have an increased risk of developing lung problems. For instance, scoliosis or problems with the structure of the chest wall may restrict a person's breathing. In addition, changes in lung tissue may increase a person's risk of developing asthma, pneumonia, emphysema, or a collapsed lung. Some people may also develop sleep apnea, a condition in which a person stops breathing periodically during sleep.
Problems during pregnancy: Women with Marfan syndrome may face complications during pregnancy. The main threat is a rapid enlargement of the aorta, which may lead to life-threatening aortic dissection or rupture. Although the risk of dissection in pregnant women is unpredictable, it is generally low if the aorta is not enlarged before pregnancy. If the aorta is even slightly enlarged in prospective mothers, however, the risk of dissection increases greatly. Pregnancy is therefore discouraged for women with enlarged aortas.
Before becoming pregnant, women with Marfan syndrome are encouraged to visit their doctors for a complete physical evaluation. Those women who do become pregnant require close monitoring throughout pregnancy. If a woman develops an enlarged aorta during pregnancy, she may need to be hospitalized or prescribed bed rest to help to reduce her blood pressure.
Treatment
General: Although Marfan syndrome is a serious and potentially life-threatening condition, it can be managed with treatment, which varies depending on individual signs and symptoms. With proper treatment, most people are able to live long, healthy lives.
Patients should be seen regularly by their doctors, including cardiologists (heart doctors), ophthalmologists (eye doctors), and primary physicians. Regular checkups are needed to monitor the patient's condition and to help prevent complications.
Back brace: Patients with scoliosis (curvature of the spine) may benefit from back braces. Although these braces do not cure scoliosis, they have been shown to prevent the condition from worsening. A brace is typically worn continuously until the patient is completely grown. During treatment, the curve may improve by as much as 50%. However, once the brace is discontinued, the spine will go back to its original curve. Children and adults who wear braces can move without much restriction.
Blood pressure-lowering drugs: A doctor may prescribe blood pressure-lowering drugs even if a person's blood pressure is normal. These medications may help to prevent the enlargement of the aorta and associated complications, which may include life-threatening aortic dissection or rupture. The most commonly prescribed drugs are called beta-blockers. They cause the heart to beat more slowly and with less force, which decreases the pressure inside the blood vessels. Side effects may include fatigue, diarrhea, and nausea.
Other blood pressure-lowering medications, such as calcium-channel blockers, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers (ARBs), may also be prescribed. Children as young as two years of age who have Marfan syndrome typically take the same medications as adults under the supervision of their doctors.
Eye surgery: The only effective treatment for a cataract is surgery to remove and replace the clouded lens with a clear lens implant. However, in some cases, cataracts are removed without inserting implant lenses. In such instances, eyeglasses or contact lenses can improve impaired vision.
Glasses or contact lenses: Many of the vision problems associated with Marfan syndrome can be corrected with glasses or contact lenses. As an alternative to lens replacement surgery, patients with dislocated lenses can wear aphakic eyeglasses and use atropine sulfate 1% ophthalmic drops, which enlarge the pupil.
Heart surgery: Some people with enlarged aortas may need to undergo surgery. If the aorta enlarges suddenly or becomes extremely large, part of the aorta and possibly the aortic valve may be surgically removed and replaced with a mechanical device or biological tissue. Tissue valves may need to be replaced after several years. If the aorta tears (called an aortic dissection) or ruptures, emergency heart surgery is needed.
Oral medications for glaucoma: If eyedrops alone do not decrease the intraocular pressure to the desired level, oral medications may also be prescribed, including the carbonic anhydrase inhibitor acetazolamide (Diamox®). Taking these medications with meals may reduce the side effects of nausea and vomiting. When an individual begins treatment with carbonic anhydrase inhibitors, he or she may frequently need to urinate and may feel a tingling sensation in the fingers and toes. After several days, these symptoms usually disappear. Other possible side effects of carbonic anhydrase inhibitors include rashes, depression, fatigue, kidney stones, lethargy, stomach upset, a metallic taste in carbonated beverages, impotence, potassium loss, and weight loss. A doctor may instruct the patient to eat bananas to help minimize the potassium deficiency that these medications can cause.
Orthopedic surgery: Orthopedic surgery may be needed for patients who develop musculoskeletal problems, such as scoliosis or a concave chest. Surgery is performed if the patient's curve is greater than a 40- to 50-degree angle. During surgery, the vertebrae along the curve are fused, or joined, together in order to straighten the spine. After surgery, the patient will remain hospitalized for several days and will spend several months in recovery. Complications may include bleeding, infection, pain, nerve damage, arthritis, and disk degeneration. If the surgery is unsuccessful, another surgery may be necessary.
If a person's chest is concave and this makes breathing difficult, surgery to raise the sternum and ribs may be recommended. This allows the lungs to expand normally and helps improve breathing.
Although a convex, or protruding, chest does not usually cause medical problems, it may be a cosmetic concern for some. Surgery is available to correct an abnormally shaped chest.
Physical activity: Depending on a person's risk of developing heart, skeletal, or eye complications, a doctor may ask a person with Marfan syndrome to avoid contact sports, such as football, field hockey, and soccer. Physical activity that puts strain on the muscles, ligaments, and heart, such as weightlifting, may also need to be avoided or limited.
However, physical activity is an important part of a healthy lifestyle. Exercise has been shown to help reduce the risk of heart disease and to improve muscle tone, which may help prevent some of the complications of Marfan syndrome. Patients should talk to their doctors to find out what exercises and activities are recommended.
Prescription eyedrops: The first line of treatment for most cases of glaucoma, except in emergency situations, is medication in the form of eyedrops. All antiglaucoma drugs work to reduce intraocular pressure. Eyedrops, such as dipivefrin (Propine®), apraclonidine (Iopidine®), and brimonidine (Alphagan®), are frequently prescribed because they tend to have fewer side effects than oral medications. Side effects vary depending on the specific medication used but may include eye redness or irritation, a change in eye color (mostly in hazel or green eyes), an increase in the thickness and number of eyelashes, headache, blurred vision, darkening of vision, joint aches, or flu-like symptoms. Eyedrops should be used as prescribed.
Shoe inserts: People with Marfan syndrome who have flat feet may benefit from shoe inserts or orthotics. These provide the feet with support and may help improve symptoms of foot pain. In addition, people are encouraged to wear comfortable, flat shoes that offer support.
Integrative Therapies
Currently, there are limited scientific data on the use of integrative therapies for the treatment or prevention of Marfan syndrome.
Prevention
There is currently no known method of preventing Marfan syndrome. Although most cases are inherited, some occur randomly.
Prenatal DNA testing may be performed if a prospective parent has Marfan syndrome. However, there are serious risks associated with prenatal testing, including miscarriage, so patients should discuss the potential health risks and benefits before making any health-related decisions.
Prospective parents with family histories of Marfan syndrome can meet with a genetic counselor to help them understanding the risks of having a child with Marfan syndrome. A genetic counselor can also explain the different types of genetic tests, including their potential risks and benefits. These counselors can also help patients understanding the results of their tests.
People who are diagnosed with Marfan syndrome should be seen regularly by their doctors, including their cardiologists (heart doctors), ophthalmologists (eye doctors), and primary physicians. Regular checkups are needed to monitor the patient's condition and to help preventing complications.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Dean JC. Marfan syndrome: clinical diagnosis and management. Eur J Hum Genet. 2007 Jul;15(7):724-33. View Abstract
Demetracopoulos CA, Sponseller PD. Spinal deformities in Marfan syndrome. Orthop Clin North Am. 2007 Oct;38(4):563-72. View Abstract.
Judge DP, Dietz HC. Therapy of Marfan syndrome. Annu Rev Med. 2007 Sep 10. View Abstract
National Heart, Lung, and Blood Institute (NHLBI). www.nhlbi.nih.gov.
National Human Genome Research Institute (NHGRI). www.genome.gov.
National Institutes of Health (NIH). www.nih.gov.
National Marfan Foundation. www.marfan.org.
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
[No authors listed.] Health supervision for children with Marfan syndrome. American Academy of Pediatrics Committee on Genetics. Pediatrics. 1996 Nov;98(5):978-82. View Abstract
Peters KF, Kong F, Hanslow M, et al. Living with Marfan syndrome III. Quality of life and reproductive planning. Clin Genet. 2002 Aug;62(2):110-20. View Abstract
Stadie R, Geipel A, Heep A, et al. Prenatal diagnosis of Marfan syndrome. Ultrasound Obstet Gynecol. 2007 Jul;30(1):119-21. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017