Liver toxicity
Liver toxicity
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Acetaminophen, aflatoxins, alanine aminotransferase, albumin, alkaline phosphatase, ALP, alpha- fetoprotein, ALT, Amanita phalloides, ammonia, APAP, ascetic, ascites, aspartate aminotransferase, Aspergillus flavus,AST, asterixis, beta-blocker, bile, biliary epithelial cells, bilirubin, cirrhosis, computerized tomography, CT, death cap mushroom, delta virus, diabetes, diuretic, drug/toxin induced hepatotoxicity, edema, endothelial cells, fatty liver, fibrosis, gallstones, hemochromatosis, hepatic cirrhosis, hepatic disorders, hepatic encephalopathy, hepatitis, hepatitis A, hepatitis B, hepatitis C, hepatitis D, hepatitis E, hepatocellular carcinoma, hepatocytes, hepatoprotection, icterus, insulin resistance, interferon, jaundice, liver transplant, mycotoxin, NAC, n-acetylcysteine, NASH, osteoporosis, pancreatitis, paracetamol, portal hypertension, sclerae, serum ferritin test, steatohepatitis, steatorrhoeic hepatosis, transferrin saturation test, type II diabetes, ultrasound, varices, viral hepatitis.
Background
The liver is the second largest organ in the body (after the skin), and is essential in keeping the body functioning properly. The liver is located in the upper right-hand side of the abdomen. It performs many functions in the body, including processing the body's nutrients, manufacturing bile to help digest fats, synthesizing many important proteins, regulating blood clotting, and breaking down potentially toxic substances into harmless ones that the body can use or excrete. Inflammation of the liver may, in severe cases, interfere with these processes and allow potentially toxic substances to accumulate. Inflammation can occur while the liver is performing its functions, such as metabolizing drugs.
The liver is able to regenerate or repair up to two-thirds of injured tissue, including hepatocytes, biliary epithelial cells, and endothelial cells. Healthy cells take over the function of damaged cells, either indefinitely or until the damage is repaired.
There are many different types of liver disease. But no matter what type the individual has, the damage to the liver is likely to progress in a similar way. Viruses cause some of them, like hepatitis A, hepatitis B, and hepatitis C. Other types of liver damage can be the result of drugs (such as acetaminophen), poisons (such as the death cap mushroom), or drinking too much alcohol for a long period of time.
If the liver forms scar tissue because of an illness, it is called cirrhosis. Jaundice, or yellowing of the skin and eyes, can be one sign of liver disease. Cancer can also affect the liver. Individuals may inherit a liver disease such as hemochromatosis, which is a liver condition causing iron overload.
According to the U.S. Centers for Disease Control and Prevention (CDC), an estimated 1.25 million Americans have chronic hepatitis (liver inflammation). About 20-30% of hepatitis patients acquired their infection during childhood. The incidence per year has declined from an average of 260,000 in the 1980s to about 60,000 in 2004. The most significant decline has occurred among children and adolescents as a result of the routine hepatitis B vaccination.
Stages of Liver Toxicity
Fatty liver and inflammation: Fatty liver, also known as steatorrhoeic hepatosis, is the build-up of excess fat in the liver cells. It is normal for the liver to contain some fat. But, if fat accounts for more than 10% of the liver's weight, the individual has fatty liver. In countries where obesity is becoming a serious health issue, fatty liver is predicted to affect approximately 25% of the general population. Fatty liver occurs before inflammation is present.
Sometimes, inflammation from a fatty liver is linked to alcohol abuse, known as alcoholic steatohepatitis. Otherwise the condition is called nonalcoholic steatohepatitis, or NASH. NASH is very common in overweight persons over the age of 30. The liver is invaded by an excessive amount of fat and a normal healthy liver tissue is partially replaced with areas of unhealthy fats. In such a liver, the liver cells and the spaces in the liver are filled with fat so that the liver becomes slightly enlarged and heavier.
Hepatitis is an inflammation of the liver that can be caused by viruses, chemicals, drugs, alcohol, inherited diseases, or the individual's own immune system. This inflammation can be acute (short-term), flaring up and then resolving within a few weeks to months, or chronic (long-term), lasting many years. Chronic hepatitis may begin to damage the liver for 20 years or more before causing significant symptoms related to progressive liver damage such as cirrhosis (scarring and loss of function), liver cancer, or death.
In the early stage of any liver disease, the liver may become inflamed, tender, and enlarged. However, an inflamed liver may cause no discomfort at all.
Fibrosis: If left untreated, the inflamed liver will start to scar. As excess scar tissue (a type of fibrous tissue) grows, it replaces healthy liver tissue. This process is called fibrosis. Scar tissue cannot function as healthy liver tissue can. Scar tissue may keep blood from flowing through the liver. The healthy part of the liver now has to work harder. The liver can regenerate, however, and may heal itself from fibrosis.
Cirrhosis: If left untreated, the liver may become so seriously scarred that it can no longer heal itself. This stage, when the damage cannot be reversed, is called cirrhosis. Cirrhosis can lead to a number of complications, including liver cancer. In some individuals, the symptoms of cirrhosis may be the first signs of liver disease. Symptoms of cirrhosis include: easy bruising; fluid buildup in the legs and/or abdomen; the skin and eyes may take on a yellow color, a condition called jaundice; the skin may itch intensely; blood may back up in vessels leading to the liver because of blockage and may burst; increased sensitivity to medications and their side effects; developing insulin resistance and type-2 diabetes; or buildup of toxins in the brain, causing problems with concentration, memory, sleeping, or other mental functions.
Liver failure: Liver failure means that the liver is losing or has lost all of its function. It is a life-threatening condition that demands urgent medical care. The first symptoms of liver failure are often nausea, loss of appetite, fatigue, and diarrhea. Because these symptoms can have any number of causes, it may be hard to tell that the liver is failing.
As liver failure progresses, the symptoms become more serious. The individual may become confused and disoriented, and extremely sleepy. There is a risk of coma and death. Immediate treatment is needed. The medical team will try to save whatever part of the liver that still works. If this is not possible, the only option may be a liver transplant.
Types and Causes of Liver Toxicity
Hepatitis: Hepatitis is a condition that impairs liver function either temporarily or permanently, sometimes leading to death. It can be initiated by a host of factors but primarily by viruses. Drugs also can cause hepatitis. However, when the specific drug is discontinued, the liver usually returns to normal.
Drug-induced: The liver is responsible for the metabolism of alcohol, drugs, and environmental toxins. It breaks them down into substances that can be used and then excreted by the body. Some drugs may cause serious injuries to the livers of patients who take them. Injuries can lead to a loss of function leading to illness, disability, hospitalization, and even life threatening liver failure and death.
Many prescription and non-prescription drugs have the potential to cause hepatitis in people, in a seemingly random fashion. The effect of drugs cannot be foreseen and the causes are unknown, although drug-induced hepatitis rarely appears to be related to an allergic reaction to the medication. Drugs that have had this affect in some people include anesthetics, antibiotics, anabolic steroids, and seizure medications. In the United States, drug-induced liver injury (DILI) is now the leading cause of acute liver failure (ALF), exceeding all other causes combined.
Acetaminophen, which is found in many over-the-counter (OTC) and prescription medications, is an example of this. In therapeutic doses, acetaminophen is a useful pain reliever, but in very high dosages or in combination with alcohol, it has the potential to cause life-threatening acute liver failure. Acetaminophen produces toxic byproducts that the liver usually detoxifies by coupling them with other compounds and flushing them out through the bile.
An estimated 500 deaths per year are attributed to suicidal or unintentional overdoses of acetaminophen (Tylenol®) as well as more than 50,000 emergency room visits. This is the most common form of acute liver failure observed in the United States. While some are intentional, at least 50% of these are unintentional; the individual is consuming more than one product containing acetaminophen or simply using doses more than suggested by the package insert.
Alcohol: The liver can metabolize only a certain amount of alcohol per hour, regardless of the amount that has been consumed. The rate of alcohol metabolism depends, in part, on the amount of metabolizing enzymes in the liver, which varies among individuals. In general, after the consumption of one standard drink, the amount of alcohol in the drinker's blood peaks within 30-45 minutes. A standard drink is defined as 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80-proof distilled spirits, all of which contain the same amount of alcohol. Alcohol is metabolized more slowly than it is absorbed. Since the metabolism of alcohol is slow, consumption needs to be controlled to prevent accumulation in the body and further intoxication. Excessive consumption of alcohol is toxic to the liver and is one of the most common causes of chemical hepatitis. Alcohol intake causes the body to overproduce an enzyme that boosts these byproducts further, while compromising the detoxification. Cirrhosis (replacement of normal tissue with scar tissue) of the liver, pancreatitis (inflammation of the pancreas), and damage to the brain and heart occur after years of heavy alcohol abuse. Heavy drinkers also are at risk of malnutrition because alcohol contains calories that may substitute for those in nutritious foods.
Fungal poisoning: When certain types of fungus grow on food, they produce minute amounts of toxins called mycotoxins. Most fungi-produced mycotoxins are harmless, and even helpful. For example, the antibiotic penicillin came from a fungus, and it is a mycotoxin. Some of these fungi (primarily Aspergillus flavus) produce the very lethal mycotoxins called aflatoxins. Aflatoxins are remarkably potent, often causing disease even when ingested in minute amounts. Aflatoxins can cause disease throughout the body, but are most commonly known for causing acute or chronic liver disease and liver cancer. Moisture, temperature, and composition of the substance the mold is on are the chief factors affecting fungal growth and aflatoxin production.
Amanita phalloides, commonly known as the death cap mushroom, is a deadly poisonous fungus (mushroom). The symptoms are slow to show themselves and often do not appear until 10-16 hours (or even longer) after eating, depending on the health of the individual and the stomach contents. Food in the stomach will increase the absorption of the toxin, causing symptoms to appear as early as six hours.
The first symptoms are stomach pains, vomiting, and diarrhea. These symptoms may continue for a day or two, after which there is typically an easing of symptoms and apparent recovery. The recovery period may last for two to three days. Then the terminal phase of three to five days starts with the re-occurrence of stomach pains, vomiting, and diarrhea accompanied by jaundice. Ingestion of the death cap mushroom can require urgent liver transplantation to save the individual's life in severe cases. Without effective, early medical intervention, coma and death occur between one and two weeks after eating the mushroom. Death is caused by liver failure, often accompanied by kidney failure.
Hepatic encephalopathy: Hepatic encephalopathy is a potentially reversible brain abnormality in the setting of liver failure, whether chronic (as in cirrhosis) or acute. It can be diagnosed only after exclusion of other neurological, psychiatric, infectious, and metabolic etiologies. Symptoms may be similar to other conditions, such as brain tumors and viral infections (including herpes simplex viruses).
With severe liver impairment, toxic substances normally removed by the liver accumulate in the blood and impair the function of brain cells. If there is also portal hypertension (high blood pressure in the portal vein inside the liver) and subsequent bypassing of the liver filtration system of blood flowing in from the intestines, these toxic substances can travel directly to the brain without being removed. Signs can include impaired cognition, a flapping tremor (asterixis), and a decreased level of consciousness including coma and, ultimately, death.
Hemochromatosis: Hemochromatosis is the most common form of iron overload disease. Primary hemochromatosis, also called hereditary hemochromatosis, is an inherited disease. Secondary hemochromatosis is caused by anemia, alcoholism, and other conditions causing liver damage. Hemochromatosis causes the body to absorb and store too much iron.
In healthy amounts, iron builds rich, red blood by helping form oxygen-carrying hemoglobin in red blood cells. Iron is also essential for a number of other body processes, including proper brain function, a strong immune system, and healthy muscles. However, excess iron stored in the body (such as in hemochromatosis) can cause health problems, such as fatigue, abdominal pain, and impotence. The extra iron can build up in the body's organs and damage them. Without treatment, the disease can cause the liver, heart, and pancreas to fail.
Juvenile hemochromatosis and neonatal hemochromatosis are two additional forms of the disease. Juvenile hemochromatosis leads to severe iron overload and liver and heart disease in adolescents and young adults between the ages of 15-30. The neonatal form causes rapid iron buildup in a baby's liver that can lead to death.
Viral hepatitis: Viruses cause most cases of hepatitis. The type of hepatitis is named for the virus that causes it, including hepatitis A, hepatitis B, hepatitis C, hepatitis D, and hepatitis E. The differences in each virus causing hepatitis include the method of transmission, symptoms, and severity.
Hepatitis A is transmitted primarily through food or water contaminated by feces from an infected person. In rare cases, it may spread via infected blood. Hepatitis A usually resolves without treatment in several weeks. However, there is a hepatitis A vaccine.
The Hepatitis B virus (HBV) causes a serious liver infection. The infection can become chronic in some people and lead to liver failure, liver cancer, cirrhosis (a condition that causes permanent scarring and damage to the liver), or death. The hepatitis B virus is transmitted through contact with bodily fluids, such as the blood and semen of someone who is infected. Even though HBV is transmitted the same way as the human immunodeficiency virus (HIV), the virus that causes AIDS, HBV is nearly 100 times as infectious as HIV. Individuals of any age, race, nationality, gender, or sexual orientation can become infected with HBV. Also, women who have HBV can transmit the infection to their babies during childbirth. When the infection is passed from mother to fetus, it is called vertical transmission. While there is no cure for HBV, the hepatitis B vaccine can prevent the disease. Also, infected individuals can take precautions to help prevent HBV from spreading to others by getting testing for the virus, abstaining from sex, using protection during sexual contact, and not sharing needles. Hepatitis B can be categorized into four different genetic groups (A through D). There is continuing research about the differences among the types. However, current findings suggest that genotype C, with its highest prevalence in Southeast Asia, is the most severe.
Hepatitis C is primarily spread via blood. It may also be transmitted through sexual contact and childbirth, although this occurs very rarely. Currently, there is no vaccine for hepatitis C. The only the way to prevent the disease is to reduce the risk of exposure to the virus. Individuals can minimize exposure to the virus by abstaining from sex, using protection during sexual contact, and not sharing needles. According to the U.S. Centers for Disease Control and Prevention (CDC), individuals who underwent hemodialysis or received blood clotting factors before 1987 are at a high risk of developing chronic hepatitis C because blood products were not tested for hepatitis C before then. Patients with acute hepatitis C should consult their healthcare providers if symptoms do not subside after two to three months.
Some evidence suggest that human leucocyte antigen (HLA) may be linked to hepatitis C. HLA are proteins that are on the outer surface of many cells in the body. The presence of two different genetic variations of HLA (HLA-DRB1*11 and HLA-DQB1*03) has been linked to a decreased incidence of developing hepatitis C-induced end-stage liver disease. In addition, a genetic marker, C4BQ0, relating to histocompatibility complex class III has been shown to be a positive risk factor for hepatitic C-related cirrhosis.
Anyone who has chronic hepatitis B is also susceptible to infection with another strain of viral hepatitis known as hepatitis D (formerly called delta virus). Hepatitis D virus can only infect cells if the hepatitis B virus (HBV) is present. Injection drug users with hepatitis B have the greatest risk of developing the infection. Individuals who are infected with both HBV and hepatitis D are more likely to develop cirrhosis or liver cancer than patients who only have HBV.
Hepatitis E is uncommon in the United States, and occurs mainly in tropical and subtropical areas. This disease is primarily spread through food or water that is contaminated by feces from an infected person. There is no vaccine for hepatitis E. The only way to prevent the disease is to reduce the risk of exposure to the virus. Hepatitis E usually resolves without treatment, within several weeks to months.
Signs and Symptoms
Jaundice is the yellowish staining of the skin and sclerae (the whites of the eyes) that is caused by high levels of the chemical bilirubin in the blood. Bilirubin is a brownish yellow substance found in bile. It is produced when the liver breaks down old red blood cells. Bilirubin is removed from the body through the stool (feces) and gives stool its normal brown color. The color of the skin and sclerae vary depending on the level of bilirubin. Excessive hemolysis or breakdown of red blood cells causes the formation of higher than normal amounts of bilirubin. When bilirubin levels increase, the liver may not be able to process the excess amounts. Jaundice then occurs. When the bilirubin level is mildly elevated, they are yellowish. When the bilirubin level is high, they tend to be brown. Icterus is the term for yellowing of the sclerae.
Other signs and symptoms of liver toxicity include: abdominal pain and swelling; chronic itchy skin; dark urine color; pale stool color; joint pain; bloody or tar-colored stool; chronic fatigue; nausea; and loss of appetite.
Complications
Edema and ascites: Fluid accumulation in the legs (edema) and in the abdomen (ascites) may occur when the liver loses its ability to make the protein albumin. Albumin, produced only in the liver, is the major plasma protein that circulates in the bloodstream.
Bruising and bleeding: Bruising and bleeding may occur when the liver slows or stops production of the proteins needed for blood clotting. The palms of the hands may be reddish and blotchy.
Itching: Bile products deposited in the skin may cause intense itching.
Gallstones: Gallstones are solid deposits of cholesterol or calcium salts that form in the gallbladder or nearby bile ducts. They often cause no symptoms and require no treatment. But some people with gallstones have a gallbladder attack (that can cause symptoms, such as nausea and an intense, steady ache in their upper middle or upper right abdomen). Gallbladder attacks include pain or tenderness under the rib cage on the right side, pain between shoulder blades, light or chalky colored stools, indigestion after eating, especially fatty or greasy foods, nausea, bloating, gas, burping or belching, and diarrhea or constipation. In some cases, the pain can be severe and intermittent.
Toxins in the blood or brain: A damaged liver cannot remove toxins from the blood, causing them to accumulate in the blood and eventually the brain. There, toxins can dull mental functioning and cause personality changes, coma, and even death. Signs of the buildup of toxins in the brain include neglect of personal appearance, unresponsiveness, forgetfulness, trouble concentrating, or changes in sleep habits.
Sensitivity to medication: Cirrhosis slows the liver's ability to filter medications from the blood. After a drug is taken, it is metabolized in the body. Metabolism is the enzymatic conversion of one chemical compound into another. Most drug metabolism occurs in the liver, although some processes occur in the gut wall, lungs, and blood plasma. Because the liver does not remove drugs from the blood at the usual rate when hepatitis is present, they act longer than expected and build up in the body. This causes a person to be more sensitive to medications and their side effects.
Portal hypertension: Normally, blood from the intestines and spleen is carried to the liver through the portal vein. But cirrhosis slows the normal flow of blood through the portal vein, which increases the pressure inside it. This condition is called portal hypertension. The portal vein may become weakened and damaged and hemorrhage (bleeding) may occur.
Varices: When blood flow through the portal vein slows, blood from the intestines and spleen backs up into blood vessels in the stomach and esophagus. These blood vessels may become enlarged because they are not meant to carry this much blood. The enlarged blood vessels, called varices, have thin walls and carry high pressure, and thus are more likely to burst. If they do burst, the result is a serious bleeding problem in the upper stomach or esophagus that requires immediate medical attention. Hemorrhages, or bleeding, may occur in damaged vessels.
Insulin resistance and type 2 diabetes: Cirrhosis causes resistance to insulin. Insulin is a hormone produced by the pancreas. Insulin enables blood glucose to be used as energy by the cells of the body. If an individual has insulin resistance, their muscle, fat, and liver cells do not use insulin properly. The pancreas tries to keep up with the demand for insulin by producing more. Eventually, the pancreas cannot keep up with the body's need for insulin, and type 2 diabetes develops as excess glucose builds up in the bloodstream.
Liver cancer: According to the National Cancer Institute (NCI), cancer of the liver is a rare malignancy in the United States, but in parts of Asia and Africa, it is one of the most common malignancies. In the United States, the average age of onset is 60-70 years, and the condition occurs more frequently in males than females by a ratio of 2:1. There is a strong association between chronic hepatitis B and C viral infections and the development of hepatocellular (liver cell) carcinoma, which account for about two-thirds of all liver cancers. People with cirrhosis also have an increased risk of liver cancer. Other possible hepatocarcinogens include aflatoxin, nitrosamines, oral estrogen and androgen compounds, and numerous other chemicals.
Ascites: Ascites is the accumulation of protein-containing (ascitic) fluid in the abdominal cavity. Ascites tends to occur in chronic (long-term) rather than in acute (short-lived) disorders. It occurs most commonly in cirrhosis (severe scarring of the liver), especially in cirrhosis caused by alcoholism or viral hepatitis. It may occur in other liver disorders, such as severe alcoholic hepatitis without cirrhosis and chronic hepatitis. Ascites can also occur in disorders unrelated to the liver, such as cancer, heart failure, kidney failure, pancreatitis (inflammation of the pancreas), and tuberculosis (a bacterial infection in the lungs) affecting the lining of the abdominal cavity. In people with a liver disorder, ascitic fluid leaks from the surface of the liver and intestine. A combination of factors is responsible. They include portal hypertension, decreased ability of the blood vessels to retain fluid, fluid retention by the kidneys, and alterations in various hormones and chemicals that regulate bodily fluids.
Problems in other organs: Cirrhosis can cause immune system dysfunction, leading to infection. Fluid in the abdomen (ascites) may become infected with bacteria normally present in the intestines. Cirrhosis can also lead to impotence, kidney dysfunction and failure, and osteoporosis.
Diagnosis
Physical examination:
History: If an acetaminophen overdosage has occurred, the doctor will attempt to determine the time and amount of acetaminophen taken. It is important for the doctor to know what medications the individual has ingested and how much. Having access to all medication bottles that the person may have taken will help the doctor to determine the maximum amount taken.
Physical: The doctor will look for signs and symptoms of liver toxicity. These signs may include jaundice (yellow skin), abdominal pain, vomiting, and ascites (fluid in the abdomen). On physical examination, a doctor looks for liver tenderness and enlargement using palpation. Palpation is a method of examination in which the examiner feels the body to determine its size, shape, firmness, or location.
Blood tests:
Albumin: Serum albumin levels measures the main protein made by the liver and tells how well the liver is making this protein. Low levels of albumin may indicate liver damage.
Ammonia: An ammonia test measures the amount of ammonia in the blood. Most ammonia in the body forms when protein is broken down by bacteria in the intestines. The liver normally converts ammonia into urea, which is then eliminated in urine. Ammonia levels in the blood rise when the liver is not able to convert ammonia to urea. This may be caused by cirrhosis or severe hepatitis.
Alpha-fetoprotein (AFP) test: Alpha-fetoprotein (AFP) is a type of protein produced in the developing embryo and fetus. In humans, AFP levels decrease gradually after birth, reaching adult levels by 8-12 months. If an individual has high levels of alpha-fetoprotein in the blood, it may be a sign of liver cancer. Healthy adult males and non-pregnant females typically have less than 40 micrograms of alpha-fetoprotein per liter of blood.
Bilirubin: Bilirubin is a waste product made from old blood cells; it is a yellow compound that causes jaundice and dark urine when present in increased amounts. Tests for bilirubin levels help determine if the liver is functioning appropriately.
INR: International normalized ratio (INR) is a blood-clotting test. It is used to measure how quickly blood forms a clot, compared with normal clotting time. The liver produces certain proteins (clotting factors) that help in blood clotting. If there is liver disease and cirrhosis, the liver may not produce the normal amount of proteins and then the blood is not able to clot normally. When a doctor is evaluating the function of the liver, a high INR usually means that the liver is not working as well as it could because it is not making the blood clot normally.
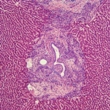
Liver biopsy: A liver biopsy may be performed to determine the extent of liver damage and to determine the best treatment option for the patient. During the procedure, a needle is inserted into the liver and a small tissue sample is removed. The tissue is then analyzed under a microscope in a laboratory.
Liver enzymes: Another blood test may be performed to check for elevated levels of liver enzymes, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST). These enzymes leak into the bloodstream when liver cells are injured. Also, alkaline phosphatase (ALP) levels may be checked. ALP is an enzyme related to the bile ducts. ALP levels are often increased when they are blocked. Liver enzymes help catalyze or start chemical reactions in the liver cells. These enzymes are released into the bloodstream when the liver is damaged.
Transferrin saturation test: The transferrin saturation test reveals how much iron is bound to the protein that carries iron in the blood. Transferrin saturation tests are used in determining if hemochromatosis exists. Transferrin saturation values higher than 45% are considered too high. The total iron binding capacity test measures how well the blood can transport iron, and the serum ferritin test shows the level of iron in the liver. If either of these tests shows higher than normal levels of iron in the body, THEN doctors can order a special blood test to detect the genetic mutation for hemochromatosis, which will confirm the diagnosis. If the mutation is not present, hereditary hemochromatosis is not the reason for the iron buildup and the doctor will look for other causes.
Diagnostic tests:
In diagnosing liver toxicity, the doctor may use images of the liver obtained by an ultrasound test, a computerized tomography (CT) scan, or a magnetic resonance imaging (MRI) scan. These diagnostic tests can determine if the presence of liver damage exists. Evidence of fatty liver or liver damage can be viewed by the doctor as dark spots or abnormal images.
A liver scan is a diagnostic procedure to evaluate the liver for suspected disease. A harmless amount of a radioactive substance that concentrates in the liver is injected intravenously (IV or into the veins) and the image of its distribution in the liver is analyzed to diagnose abnormalities. Women who are pregnant or breastfeeding should not have this test.
Treatment
General: Therapies for liver toxicity focus on reducing the complications of the disease.
Individuals who knowingly have been exposed to the hepatitis B virus (HBV) should consult their healthcare providers as soon as possible. Patients who receive an injection of hepatitis B immune globulin within 24 hours of exposure to the virus may not develop HBV infection. Patients should also receive the first of three injections of the hepatitis B vaccine.
Diuretics:Diuretics, or fluid tablets, are used in the treatment of fluid retention in the legs (edema) or abdomen (ascites).
Laxatives: Laxatives, such as lactulose (Chronulac®), are used to prevent constipation and to reduce the chances of the poisonous substances, such as ammonia, from the bowel bypassing the liver and reaching the brain, causing drowsiness, confusion, and coma (hepatic encephalopathy).
Weight loss and exercise: If the individual's body mass index (BMI) is above 25, a diet and exercise program may reduce the amount of accumulated fat in the liver. BMI measures the amount of fat the body contains. The most effective diet is rich in fiber and low in calories and saturated fat, with total fat accounting for no more than 30% of total calories.
Diabetes control: Strict management of diabetes with diet, medications, or insulin lowers blood sugar, which may prevent further liver damage. Blood sugar control may also reduce the amount of accumulated fat in the liver.
Cholesterol control: Controlling elevated levels of cholesterol and triglycerides with diet, exercise, and cholesterol-lowering medications may help stabilize or reverse nonalcoholic fatty liver disease.
Avoidance of toxic substances: If an individual has nonalcoholic fatty liver disease, especially nonalcoholic steatohepatitis (NASH), alcohol should not be consumed. Medications and other substances that can cause liver damage should also be avoided, such as acetaminophen (Tylenol®).
Ursodiol (Actigall®): Ursodiol (Actigall®) is a prescription medication most commonly used to treat gallstones. Ursodiol decreases production of bile acids, which may in theory help lower elevated levels of liver enzymes in individuals with liver disease.
Beta-blockers: For portal hypertension, the doctor may prescribe a beta blocker, such as propranolol (Inderal®). These drugs are normally used in hypertension or high blood pressure. Side effects include fatigue and loss of sexual desire.
N-acetyl cysteine (NAC): The antidote to acetaminophen overdose is N-acetylcysteine (NAC). NAC is most effective when given within eight hours of ingesting acetaminophen. Indeed, NAC can prevent liver failure if given early enough. For this reason, it is absolutely necessary that acetaminophen poisoning be recognized, diagnosed, and treated as early as possible. NAC can be purchase over-the-counter (OTC) as a dietary supplement, but when used for acetaminophen toxicity, NAC is a concentrated solution that is prescribed by a doctor and mixed appropriately by a pharmacist.
Other medications: Researchers are studying the effects of several medications on insulin resistance and nonalcoholic fatty liver disease in individuals with and without diabetes. These include metformin (Glucophage®, Glucophage XR®), pioglitazone (Actos®), rosiglitazone (Avandia®), and betaine (Cystadane®). Another drug being investigated is orlistat (Xenical®), a medication that blocks the absorption of some of the fat from food. Early results indicate that orlistat may reduce the amount of fat in the liver.
Interferon: Interferons are natural proteins produced by the cells of the immune system in response to challenges by foreign agents such as viruses, bacteria, parasites, and tumor cells. Administering additional synthetic interferon may stimulate the body's immune response to hepatitis B virus (HBV) and help prevent the virus from spreading. Two interferon medications are available: interferon alfa-2b (Intron A®) and peginterferon alfa-2a (Pegasys®). Intron A® is administered by injection several times a week. Pegasys® is given by injection once a week.
Not everyone is a candidate for interferon treatment. In a few cases, interferon has successfully eliminated the virus completely. However, the infection can return in the future. Several side effects are associated with interferon, including depression, fatigue, muscle pain, body aches, fever, and nausea. Interferon may also cause a decreased production of red blood cells. Symptoms are usually worse during the first two weeks of treatment and in the first four to six hours after receiving an injection of interferon.
Lamivudine (Epivir-HBV®): Lamivudine (Epivir-HBV®) is an antiviral medication that helps prevent HBV from replicating in the body's cells. The medication is usually taken in tablet form once daily. Side effects during treatment are generally mild, but some patients may experience a severe worsening of symptoms when they stop taking the medication. Patients should tell their healthcare providers if they have had any kidney problems or history of pancreatitis before starting this medication. Patients should call their healthcare providers immediately if they experience a worsening of jaundice (yellowing of the skin and eyes) or if they experience any unusual bruising, bleeding, or fatigue while taking the medication.
Adefovir dipivoxil (Hepsera®): Adefovir dipivoxil (Hepsera®) is a tablet taken orally once a day to help prevent HBV from replicating inside the body's cells. This drug is effective in patients who are resistant to lamivudine. Like lamivudine, side effects are generally mild, but symptoms may worsen when treatment is stopped. Hepsera® may cause kidney toxicity in patients with underlying kidney disease. A change in the amount of urine produced or blood in the urine may indicate kidney toxicity. Other side effects may include weakness, headache, fever, increased cough, nausea, vomiting, diarrhea, or gas.
Entecavir (Baraclude®): Entecavir (Baraclude®) is an antiviral medication that was approved by the U.S. Food and Drug Administration (FDA) in March 2005 for HPV (human papilloma virus). HPV infection is a sexually transmitted disease that may lead to cervical cancer in women. This medication is taken orally once a day. Studies comparing entecavir to lamivudine in hepatitis treatment found that entecavir was more effective. Baraclude® may cause symptoms of hepatitis to worsen once medication is discontinued.
Liver transplant: When the liver has been severely damaged, a liver transplant may be the only treatment option. Liver transplants are increasingly successful. However, there are not enough donor organs available for every patient who needs a transplant, and not all patients are suitable transplant candidates. It is estimated that more than 10,000 living donor transplants have been performed worldwide, and that the donor recipient death rate ranges from 0.1-0.3%.
Integrative Therapies
Strong scientific evidence:
N-acetyl cysteine: Strong scientific evidence supports the use of N-acetyl cysteine (NAC) as an antidote to acetaminophen overdose. Acetaminophen metabolism causes an increased demand for glutathione. NAC supports glutathione synthesis, in particular when the need for glutathione increases.
Use with caution in patients with bleeding disorders or taking drugs that may increase the risk of bleeding, in patients with blood pressure disorders or taking agents that affect blood pressure, or in patients with diabetes, high or low blood sugar, or taking agents that affect blood sugar. Use with caution in patients with heart disease, gastrointestinal disorders, breathing disorders, zinc deficiency, unpleasant mood, or those complaining of dizziness, lightheadedness, or visual complaints. Use with caution in those using antibiotics, nitroglycerin, or needing charcoal treatment. Avoid in doses greater than 30 grams daily. Avoid in pregnant or breastfeeding women. Avoid with known allergy or sensitivity to NAC or related substances.
Good scientific evidence:
Betaine: Betaine is found in most microorganisms, plants, and marine animals. Its main physiologic functions are to protect cells under stress and as a source of methyl groups needed for many biochemical pathways. Betaine is also found naturally in many foods and is most highly concentrated in beets, spinach, grain, and shellfish. Betaine raises S-adenosylmethionine (SAM) levels that may in turn play a role in improving hepatic steatosis, or fatty liver.
Avoid if allergic or hypersensitive to betaine or a type of betaine called cocamidopropylbetaine. Use cautiously with kidney disease, obesity, or psychiatric conditions. Avoid if pregnant or breastfeeding.
Cordyceps: In traditional Chinese medicine, cordyceps has been used to support and improve liver function. Cordyceps may stimulate the immune system and improve serum gamma globulin levels in hepatitis B patients. Currently, there is insufficient evidence to recommend for or against the use of cordyceps for chronic hepatitis B. However, early study results are promising. Additional research of cordyceps and current hepatitis treatments is needed.
Avoid if allergic or hypersensitive to cordyceps, mold or fungi. Use cautiously with diabetes, bleeding disorders or taking anticoagulant medications, with prostate conditions, if taking immunosuppressive medications, or if on hormonal replacement therapy or oral contraceptives. Avoid with myelogenous type cancers. Avoid if pregnant or breastfeeding.
Milk thistle: Multiple studies from Europe suggest benefits of oral milk thistle for cirrhosis. In experiments up to five years long, milk thistle has improved liver function and decreased the number of deaths that occur in cirrhotic patients. Although these results are promising, most studies have been poorly designed. Further research is necessary before a strong recommendation can be made.
In addition, several studies of oral milk thistle for chronic hepatitis caused by viruses or alcohol report improvements in liver tests. However, most studies have been small and poorly designed. More research is needed before a recommendation can be made.
Use cautiously if allergic to plants in the aster family (Compositea, Asteraceae), daisies, artichoke, common thistle, or kiwi. Use cautiously with diabetes. Avoid if pregnant or breastfeeding.
Molybdenum: Wilson's disease is an inherited disorder of copper metabolism characterized by a failure of the liver to excrete copper, which leads to its accumulation in the liver, brain, cornea, and kidney, with resulting chronic degenerative changes. Tetrathiomolybdate (TM), a form of molybdenum, has been studied for use in diseases involving copper metabolism, such as Wilson's disease. At this time, evidence in support of TM for Wilson's disease is inconclusive. Further research is warranted.
Use with caution in patients with copper deficiency, those at risk of copper deficiency, or patients with metabolic disorders that decrease copper. Use with caution in patients with diabetes or hypoglycemia and in those taking drugs, herbs, or supplements that affect blood sugar. Use with caution in patients with low blood pressure or in those taking agents that lower blood pressure. Use with caution in patients with phenylketonuria who require a semisynthetic phenylalanine-restricted diet; those with gout, lipid disorders, of kidney disorders; or premature infants, unless under the care of a physician. Use with caution at high doses with sulfur-containing agents. Avoid in doses exceeding the tolerable upper intake level. Avoid in patients with allergies or hypersensitivity to molybdenum or its constituents. Avoid use of tetrathiomolybdate (TM), a form of molybdenum, unless under the care of a physician. Avoid levels greater than those commonly found in multivitamin and mineral supplements if pregnant or breastfeeding.
Probiotics: Liver cirrhosis may be accompanied by an imbalance of intestinal bacteria flora. Probiotic supplementation in cirrhosis patients has been found to reduce the level of fecal acidity (pH) and fecal and blood ammonia, which are beneficial changes.
Probiotics are generally considered safe and well tolerated. Avoid if allergic or hypersensitive to probiotics. Use cautiously if lactose intolerant.
Zinc: Early research suggests that zinc treatment may be effective in the management of Wilson's disease. More well-designed trials are needed to confirm these early results.
Zinc is generally considered safe when taken at the recommended dosages. Avoid zinc chloride since studies have not been done on its safety or effectiveness. While zinc appears safe during pregnancy in amounts lower than the established upper intake level, caution should be used since studies cannot rule out the possibility of harm to the fetus.
Unclear or conflicting scientific evidence:
Acidophilus: Lactobacilli are bacteria that normally live in the human small intestine and vagina.There is limited study in individuals with hepatic encephalopathy (confused thinking due to liver disorders), and more studies need to be performed in this area.
Acidophilus may be difficult to tolerate if allergic to dairy products containing L. acidophilus. Avoid with history of an injury or illness of the intestinal wall, immune-disease, or heart valve surgery. Avoid with prescription drugs, like corticosteroids, because of the risk of infection. Use cautiously with heart murmurs. Antibiotics or alcohol may destroy Lactobacillus acidophilus. Therefore, it is recommended that Lactobacillus acidophilus be taken three hours after taking antibiotics or drinking alcohol. Some individuals can use antacids (like famotidine (Pepcid®), esomeprazole (Nexium®)) to decrease the amount of acid in the stomach one hour before taking Lactobacillus acidophilus.
Alpha-lipoic acid: Alpha-lipoic acid (ALA) has been studied as a treatment for alcoholic liver disease. However, benefits have not been observed at this time. More research is needed in this area.
Avoid if allergic to ALA. Use cautiously with diabetes and thyroid diseases. Avoid with thiamine deficiency or alcoholism. Avoid if pregnant or breastfeeding.
Astragalus: Anti-viral activity has been reported with the use of astragalus in laboratory and animal studies. Limited human and animal research has examined the use of astragalus for viral infections in the liver (hepatitis B and C). However, most studies have been small and poorly designed. Due to a lack of well-designed research, no firm conclusions can be drawn. Clinical data suggests that astragalus may be effective in treating cirrhosis. Further research is needed to better understand the use of astragalus for liver protection.
Avoid if allergic to astragalus, peas, or any related plants or with a history of Quillaja bark-induced asthma. Avoid with aspirin or aspirin products or herbs or supplements with similar effects. Avoid with inflammation (swelling) or fever, stroke, transplant or autoimmune diseases (like HIV/AIDS). Stop use two weeks before surgery/dental/diagnostic procedures with a risk of bleeding and avoid use immediately after these procedures. Use cautiously with bleeding disorders, diabetes, high blood pressure, lipid disorders, or kidney disorders. Use cautiously with blood-thinners, blood sugar drugs, or diuretics or herbs and supplements with similar effects. Avoid if pregnant or breastfeeding.
Ayurveda: Ayurveda is an integrated system of specific theories and techniques employing diet, herbs, exercise, meditation, yoga and massage or bodywork. Clinical evidence suggests that the traditional herbal preparation Kamalahar may reduce clinical signs as well as indicators of liver damage in acute viral hepatitis. Kamalahar contains Tecoma undulate, Phyllanthus urinaria, Embelia ribes, Taraxacum officinale, Nyctanthes arbortistis, and Terminalia arjuna. The root powder from the herb Picrorhiza kurroa has also been shown to improve levels of bilirubin, SGOT (serum glutamic-oxaloacetic transaminase) and serum glutamic pyruvic transaminase (SGPT) in viral hepatitis. Further research is needed before a firm conclusion can be made.
Ayurvedic herbs should be used cautiously because they are potent and some constituents can be potentially toxic if taken in large amounts or for a long time. Some herbs imported from India have been reported to contain high levels of toxic metals. Ayurvedic herbs can interact with other herbs, foods and drugs. A qualified healthcare professional should be consulted before taking.
Biotin: Biotin is an essential water-soluble B vitamin. Antioxidant therapy with biotin, vitamins A-E, selenium, zinc, manganese, copper, magnesium, folic acid, and coenzyme Q10 was not shown to improve survival rates for hepatitis. More research with biotin alone is needed.
Biotin is a water-soluble vitamin required in the human diet. Biotin is likely safe at levels typically found in food and in cosmetic formulations. Doses 600-fold greater than the estimated daily intake are considered safe. Adverse effects, even at high doses, are minor or absent. Use cautiously in patients taking anticonvulsants, antibiotics, agents that are processed by the liver, or isotretinoin (Roaccutane®). Use cautiously in pregnant or breastfeeding women. Marginal biotin deficiency may develop during normal pregnancy and cause birth defects. Eating large amounts of raw egg white over time is likely to result in biotin deficiency. Smoking may cause marginal biotin deficiency in women. Reports of allergy or anaphylaxis to biotin supplementation are rare.
Bupleurum: For more than 2,000 years bupleurum has been used in Asia to treat hepatitis, cirrhosis and other conditions associated with inflammation. A high-quality clinical trial and several small recent clinical reports suggest that bupleurum and/or an herbal combination formula containing bupleurum may be helpful in the treatment of chronic hepatitis. However, studies to date are small and not all well controlled. Further research is warranted to determine whether bupleurum can effectively treat hepatitis.
Avoid if allergic or hypersensitive to bupleurum, Apiaceae or Umbelliferae (carrot) families, snakeroot, cow parsnip, or poison hemlock. Use cautiously if operating motor vehicles or hazardous machinery. Use cautiously with low blood pressure, diabetes, or edema. Use cautiously with a history of bleeding, hemostatic disorders, or drug-related hemostatic disorders. Use cautiously if taking blood thinners. Avoid if pregnant or breastfeeding.
Capers: There is limited evidence of the effect of capers alone on cirrhosis. Additional studies are needed.
Capers are generally considered to be safe. Avoid with allergy or sensitivity to capers or mustard oil. There are limited reports of side effects with capers. Use cautiously with diabetes or low blood sugar or in those taking drugs, herbs, or supplements that lower blood sugar. Use cautiously with low blood pressure or if taking drugs, herbs, or supplements that lower blood pressure. Use cautiously in patients prone to iron overload. Use cautiously if taking diuretics. Use cautiously if pregnant or breastfeeding.
Chicory: Chicory (Chichorium intybus) has been suggested as a possible treatment for chronic hepatitis. However, further research is needed before a definitive conclusion can be made.
Avoid if allergic/hypersensitive to chicory or members of the Asteraceae or Compositae family, including ragweed, chrysanthemums, marigolds, and daisies. Use cautiously if taking drugs or herbs metabolized by cytochrome P450 enzymes. Use cautiously with gallstones. Avoid if pregnant or breastfeeding.
Chlorophyll: Chlorophyll is a chemoprotein commonly known for its contribution to the green pigmentation in plants, and is related to protoheme, the red pigment of blood. It can be obtained from green leafy vegetables (broccoli, Brussel sprouts, cabbage, lettuce, and spinach), algae (Chlorella and Spirulina), wheat grass, and numerous herbs (alfalfa, damiana, nettle, and parsley). Laboratory evidence suggests chlorophyll may be of use as a chemopreventative agent due to its potential ability to inhibit the tumor-promoting effects of carcinogens. Chlorophyll may act to improve the detoxification of toxins involved in cancer promotion. However, more research is needed in regard to protection from aflatoxins. It may also inhibit the absorption of dietary heterocyclic aromatic amines, which may act as potential carcinogens. The results of one clinical trial suggest that prophylactic interventions with chlorophyllin or diet supplementation with chlorophyll-rich foods may be a practical means to prevent the development of hepatocellular carcinoma or other environmentally-induced cancers. Additional large scale clinical research is needed in this area before a clinical recommendation can be made.
Avoid if allergic or hypersensitive to chlorophyll or any of its metabolites. Use cautiously with photosensitivity, compromised liver function, diabetes or gastrointestinal conditions or obstructions. Use cautiously if taking immunosuppressant agents or antidiabetic agents. Avoid if pregnant or breastfeeding.
Choline: Studies have assessed the use of choline for acute viral hepatitis, many of which have been poorly designed. There is currently insufficient evidence available to determine whether choline can effectively treat hepatitis.
Avoid if allergic/hypersensitive to choline, lecithin, or phosphatidylcholine. Use cautiously with kidney or liver disorders or trimethylaminuria. Use cautiously with a history of depression. If pregnant or breastfeeding it seems generally safe to consume choline within the recommended adequate intake (AI) parameters; supplementation outside of dietary intake is usually not necessary if a healthy diet is consumed.
Clay: Phyllosilicate clay has been shown to adhere to aflatoxins in laboratory study, and HSACS clay in animal diets may diminish or block exposure to aflatoxins. However, the risks of chronic clay exposure likely do not justify the potential benefit of protection from aflatoxins.
There is a lack of reports of allergy to clay in the available scientific literature. However, in theory, allergy/hypersensitivity to clay, clay products, or constituents of clay may occur. Avoid if pregnant or breastfeeding.
Cordyceps: In traditional Chinese medicine, cordyceps has been used to support and improve liver function. In two studies using herbal combinations that included cordyceps, liver and immune function were improved. However, as these studies used combination treatments, the effect of cordyceps alone for treatment of cirrhosis is currently unknown.
Avoid if allergic or hypersensitive to cordyceps, mold or fungi. Use cautiously with diabetes, bleeding disorders or taking anticoagulant medications, with prostate conditions, if taking immunosuppressive medications, or if on hormonal replacement therapy or oral contraceptives. Avoid with myelogenous type cancers. Avoid if pregnant or breastfeeding.
Dandelion: Human study reports improved liver function in patients with chronic hepatitis B after taking a combination herbal preparation containing dandelion root, called Jiedu Yanggan Gao (also including Artemisia capillaris, Taraxacum mongolicum, Plantago seed, Cephalanoplos segetum, Hedyotis diffusa, Flos chrysanthemi indici, Smilax glabra, Astragalus membranaceus, Salviae miltiorrhizae, Fructus polygonii orientalis, Radix paeoniae alba, and Polygonatum sibiricum). Because multiple herbs were used the effects of dandelion are unclear.
Avoid if allergic to chamomile, feverfew, honey, yarrow, or any related plants such as aster, daisies, sunflower, chrysanthemum, mugwort, ragweed, or ragwort. Use cautiously with diabetes or bleeding disorders, gastroesophageal reflux disease (GERD), kidney or liver diseases, or a history of stroke or electrolyte disorders. Potassium blood levels should be monitored. Stop use two weeks before surgery/dental/diagnostic procedures with bleeding risk and do not use immediately after these procedures. Avoid if pregnant or breastfeeding.
Danshen: Some studies suggest that danshen may provide benefits for treating liver diseases such as cirrhosis, fibrosis and hepatitis B. However, it is unclear whether there are any clinically significant effects of danshen in patients with these conditions.
Avoid if allergic or hypersensitive to danshen. Use cautiously with altered immune states, arrhythmia, compromised liver function or a history of glaucoma, stroke, or ulcers. Stop use two weeks before surgery/dental/diagnostic procedures with bleeding risk, and do not use immediately after these procedures. Use cautiously if driving or operating heavy machinery. Avoid if taking blood thinners (anticoagulants), digoxin or hypotensives including ACE inhibitors such as captopril, or Sophora subprostrata root or herba serissae. Avoid with bleeding disorders, low blood pressure and following cerebal ischemia. Avoid if pregnant or breastfeeding.
Docosahexaenoic acid (DHA): Salmon roe phospholipids, a third of which consisted of DHA, have been found to beneficial in patients with liver disease. In preliminary research, DHA improved fatty liver severity and insulin sensitivity in children with nonalcoholic fatty liver disease (NAFLD). Further research is needed before conclusions may be drawn.
Use cautiously in patients with high cholesterol, diabetes, anxiety, sexual dysfunction, autoimmune disorders, heart rate abnormalities, or in those taking heart rate-regulating agents, anticoagulants, antiplatelets, blood pressure lowering agents, antilipemics, or agents that affect the immune system. Use cautiously in couples trying to get pregnant, especially in men with a low sperm count. Researchers caution against DHA supplementation, in the absence of AA supplementation, during the first two trimesters of pregnancy. Avoid in patients with known allergy or hypersensitivity to fish, fish oils, or any marine products.
Eyebright: Limited evidence from animal studies suggests that aucubin, a constituent of eyebright, may inhibit hepatic RNA and protein syntheses in vivo. These properties have been associated with protective effects in carbon tetrachloride and alpha-amanitin-induced hepatotoxicity in mice. Conversion of aucubin to its algycone appears to be a prerequisite step for these hepatic effects to occur. The clinical relevance of these finding to humans is unclear, and there is currently insufficient evidence to determine whether eyebright is an effective agent for hepatoprotection.
Avoid if allergic to eyebright, any of its constituents, or members of the Scrophulariaceae family. Use cautiously with diabetes and drugs that are broken down by the liver. Avoid if pregnant or breastfeeding.
Germanium: There is limited evidence for the use of propagermanium (an organogermanium) in the treatment of hepatitis B. Additional research is warranted in this area.
Avoid if allergic or hypersensitive to germanium, its compounds or germanium-containing plants. Avoid if pregnant or breastfeeding.
Ginseng: There is currently a lack of sufficient evidence to recommend either American ginseng or Panax ginseng as an agent for liver protection. Laboratory study investigated compound K, a ginseng metabolite that shows promise in protecting against liver injury. Additional human studies are warranted in this area. Early studies show that ginseng may improve some aspects of liver function but not others. More research is needed regarding chronic hepatitis B.
Avoid with known allergy to plants in the Araliaceae family. There has been a report of a serious life-threatening skin reaction, possibly caused by contaminants in ginseng formulations.
Gotu kola: Study results of gotu kola (Centella asiatica) for liver disease are mixed. Further research is needed before a recommendation can be made for liver cirrhosis.
Avoid if allergic to gotu kola, asiaticoside, asiatic acid, or madecassic acid. Avoid with a history of high cholesterol, cancer, or diabetes. Avoid if pregnant or breastfeeding.
Green tea: Limited study suggests that green tea may reduce the risk of liver disease. Additional research is necessary before a conclusion can be made.
Use with caution with alcohol, antifungals, birth control pills, decongestants, and diuretics, and in patients with blood disorders, cardiovascular disorders, breast disease, an empty stomach, eye disorders, gastrointestinal disorders, impaired iron metabolism, iron deficiency, liver disorders, or psychiatric disorders. Use with caution in postmenopausal women; those prone to headaches, those at risk for prostate cancer or osteoporosis. Use with caution in patients using agents to treat eye disorders; agents that affect the gastrointestinal system; agents that affect hormone levels, agents that may damage the liver, or agents that affect the nervous system, as well as when using iron, painkillers, and other agents containing caffeine. Use of green tea extract Polyphenon E® ointment may result in skin irritation or sun sensitivity. Avoid taking in excessively high amounts by mouth; during pregnancy and breast feeding; with known allergy or sensitivity to green tea, its constituents, caffeine, tannins, or members of the Theaceae family.
Ipecac: In several studies, ipecac was shown to be effective in reducing acetaminophen (e.g., Tylenol®) concentration when administered within 30 minutes or less after acetaminophen overdose. More studies are needed.
A watery extract of ipecac is reportedly many times stronger than syrup of ipecac; as little as 10 milliliters of fluid extract may be fatal. Drowsiness may occur; use with caution when driving or operating heavy machinery. Ipecac abuse may result in heart failure and death. Cases of pneumonia have occurred after giving ipecac and activated charcoal. Vomiting produced by ipecac may reduce the effects of many drugs, herbs, or supplements if given within one hour of taking the drug, herb, or supplement. Agents that inhibit vomiting may decrease vomiting in patients who have ingested ipecac. Use cautiously in children under 12 years of age and the elderly. Avoid in patients who have a depressed mental status or gag reflex, a history of Münchausen syndrome, a history of eating disorders, a history of susceptibility to bleeding, or a history of Mallory-Weiss syndrome (bleeding from the junction of the esophagus and stomach following a vomiting episode). Avoid in patients who have ingested a sharp foreign object, a toxin that may cause seizures, a strong acid, a strong alkali, a tricyclic antidepressant, camphor, cocaine, heroin, a hydrocarbon, or strychnine. Avoid in patients who are under six months of age. Avoid during pregnancy and breastfeeding or with known allergy or sensitivity to ipecac.
L-carnitine: Although early evidence suggests that L-carnitine may effectively treat cirrhosis, further research is needed to confirm these results. Preliminary evidence also suggests that L-carnitine may be of benefit to individuals with hepatic encephalopathy, in terms of ammonia levels and psychometric functioning. Additional study is needed.
Avoid with known allergy or hypersensitivity to carnitine. Use cautiously with peripheral vascular disease, hypertension (high blood pressure), alcohol-induced liver cirrhosis, and diabetes. Use cautiously in low birth weight infants and individuals on hemodialysis. Use cautiously if taking anticoagulants (blood thinners), beta-blockers, or calcium channel blockers. Avoid if pregnant or breastfeeding.
Lecithin: Although not well studied in humans, lecithin has been shown to have liver-protecting effects. Positive results have been seen when lecithin was given to patients with chronic hepatitis who had also received drugs to reduce the activity of the immune system. Further studies are needed before a conclusion can be made.
Lecithin is generally well tolerated. Although human research is limited, lecithin may have toxic effects on the liver. Use cautiously in patients with liver disease, those with bleeding disorders, and patients taking agents for these conditions. Avoid with known allergy or hypersensitivity to lecithin, egg, or soy. There is currently a lack of available scientific evidence on the use of lecithin in pregnant or breastfeeding women.
Licorice: The licorice extracts DGL and carbenoxolone have been proposed as possible therapies for viral hepatitis. Further research is needed before a firm conclusion can be made.
Avoid with a known allergy to licorice, any component of licorice, or any member of the Fabaceae (Leguminosae) plant family. Avoid with congestive heart failure, coronary heart disease, kidney or liver disease, fluid retention, high blood pressure, hormonal abnormalities or if taking diuretics. Licorice can cause abnormally low testosterone levels in men or high prolactin or estrogen levels in women. This may make it difficult to become pregnant and may cause menstrual abnormalities.
Liver extract: Liver extract seems to stimulate liver function and may be of benefit in treatment of hepatic disorders such as chronic hepatitis. More research is needed to compare liver extract to other hepatostimulatory treatments.
Avoid if allergic or hypersensitive to liver extract or its constituents. Use cautiously if taking antacids or with acid reflux. Use cautiously with clotting disorders, compromised immune function, and abnormal iron levels. Use cautiously if taking antihypercholesterolemic drugs (drugs that affect blood cholesterol), antiviral agents, especially interferon, or any agents for cancer. Use cautiously as raw liver may contain liver flukes or the bacterium, Vibrio fetus. Use cautiously in hepatopathic patients with reduced human growth hormone metabolic clearance rate. Avoid liver extract with iron metabolism disorders or iron shortage disorders, such as hemochromatosis. Avoid liver extract from countries where bovine spongiform encephalitis (BSE or "mad cow disease") has been reported. Avoid if sensitive to liver extract or any of its components, as liver extract therapy has caused severe anaphylactic shock. Avoid if pregnant or breastfeeding.
Manganese: N-acetyl cysteine, vitamins A-E, biotin, selenium, zinc, manganese, copper, magnesium, folic acid, and coenzyme Q in combination showed a lack of effect on alcoholic hepatitis. Additional studies are needed in this area.
Manganese is likely safe in levels commonly found in the diet. Manganese may affect fertility, although this has not been well studied in humans. Use cautiously in patients with non-Hodgkin's lymphoma, ileal pouch-anal anastomosis, and malignancies, and in total parenteral nutrition. Avoid in patients with chronic liver disease who are receiving parenteral nutrition, in patients with iron-deficiency anemia, and in patients with heart disease. Avoid with known allergy or hypersensitivity to manganese. Avoid long-term exposure to manganese. Long-term exposure and high manganese levels in the body may lead to psychiatric and motor disturbances (termed manganism) and may be a risk factor for the development of various disorders that affect the brain and nervous system.
Methionine: Several studies have investigated the use of methionine for treatment of acetaminophen (e.g., Tylenol®) overdose. In a study of patients with acetaminophen poisoning, methionine worked as well as standard treatment with acetylcysteine in preventing major liver damage and death. Further study is required before any conclusion can be made.
Use cautiously in individuals taking gastrointestinal agents. Use cautiously in patients who have or are at risk for elevated homocysteine levels or who are using agents that may elevate homocysteine levels (e.g., antiseizure agents, fenofibrate, niacin). Use cautiously in infants receiving parenteral (put into the body other than via the digestive tract) nutrition with methionine, particularly in large amounts, due to increased risk of liver injury. Use cautiously in individuals with liver disease or those who are taking drugs, herbs, or supplements that may damage the liver. Avoid large amounts of methionine (more than 100 milligrams per kilogram of body weight), as it may lead to severe brain effects.
Milk thistle: Milk thistle (Silybum marianum) has been used medicinally for over 2,000 years, most commonly for the treatment of liver and gallbladder disorders. Several clinical studies suggest possible benefits of milk thistle to treat or prevent drug or toxin induced liver toxicity. Results of this research are not clear, and most studies have been poorly designed. More research needs to be performed in this area. Milk thistle has been used traditionally to treat Amanita phalloides mushroom toxicity and poisoning. However, there are not enough reliable studies in humans to support this use of milk thistle. Research on milk thistle for acute viral hepatitis has not provided clear results, and milk thistle cannot be recommended for this potentially life-threatening condition at this time.
Caution is advised when taking milk thistle supplements, as numerous adverse effects including an increased risk of bleeding and drug interactions are possible. Milk thistle should not be used during pregnancy or breastfeeding unless otherwise directed by a doctor.
Mistletoe: In preliminary research, some patients achieved complete elimination of the hepatitis virus after treatment with Viscum album, although these studies were not well designed. A small exploratory trial investigated effects of mistletoe on liver function, reduction of viral load and inflammation, and maintaining quality of life by the immunomodulatory and/or cytotoxic actions of mistletoe extracts, but little effect was seen. Larger, well-designed clinical trials are needed to resolve this conflicting data.
Avoid if allergic to plants in the aster family (Compositea, Asteraceae), daisies, artichoke, common thistle, or kiwi. Use cautiously with diabetes. Avoid if pregnant or breastfeeding.
Peony: The peony species Paeonia lactiflora Pallas has been used in traditional Chinese medicine (TCM) to treat liver disease. In humans, Paeonia rubra root has been given to patients with liver cirrhosis. Larger controlled trials of higher methodological quality are necessary to substantiate the positive results of this small case series.
Avoid if allergic or sensitive to peony. Avoid with bleeding disorders or if taking drugs, herbs, or supplements that increase bleeding risk. Use cautiously with estrogen-sensitive cancers or if taking drugs, herbs, or supplements with hormonal activity. Avoid if pregnant or breastfeeding.
Phosphatidylcholine: Preliminary research suggests that phosphatidylcholine may be useful in the treatment of liver failure. Limited research suggests that phosphatidylcholine, in combination with interferon, may be useful in the treatment of some forms of chronic hepatitis. Further research is needed before a conclusion can be made.
Injectable phosphatidylcholine should only be administered by a qualified healthcare provider. Use cautiously in patients with gastrointestinal disorders. Avoid in pregnant or breastfeeding women or in subjects with known allergy or sensitivity to phosphatidylcholine.
Probiotics: Initial studies of probiotics for minimal hepatic encephalopathy (confused thinking due to liver disorders) are encouraging. Probiotics and probiotics may lead to the improvement of symptoms and may be an alternative to lactulose for the management of this condition in people with cirrhosis. However, more studies are needed to determine the role of probiotics in this condition.
Probiotics are generally considered safe and well-tolerated. Avoid if allergic or hypersensitive to probiotics. Use cautiously if lactose intolerant.
PSK: PSK, or protein-bound polysaccharide, is obtained from cultured mycelia of the Coriolus versicolor, a mushroom thought to have antimicrobial, antiviral, and antitumor properties. Studies of PSK as a therapy for liver cancer have yielded mixed results. Well-designed clinical trials are needed to determine the role of PSK on survival time and remission in patients with liver cancer.
PSK generally seems to have a low incidence of mild and tolerable side effects. In one report, three cases of toxicity were noted, and PSK was discontinued. PSK has been associated with side effects of gastrointestinal upsetand darkening of the fingernails, but these effects have been limited and general safety has been demonstrated with daily oral doses for extended periods. Darkening of the fingernails and coughing have been reported during administration of the powdered form of PSK.
Pyruvate: Preliminary study suggests that sodium pyruvate infusions decrease levels of various liver function tests in patients with alcoholic liver disease. Well-designed, randomized clinical trials are required before conclusions may be drawn.
Use cautiously in patients with cardiomyopathy, gastrointestinal disorders, or in those taking medications that may affect blood pressure, or antilipemics, cardiovascular agents, or insulin. Avoid in patients with a known allergy or hypersensitivity to pyruvate or its constituents. Avoid in pregnant or lactating women or in children, due to a lack of sufficient safety data.
Reishi mushroom: Based on positive laboratory evidence, a clinical trial using Ganopoly® or placebo was conducted in chronic hepatitis B patients. Ganopoly® treatment decreased levels of hepatitis B virus (HBV) DNA. Further well-designed research is needed before a firm conclusion can be made.
Avoid if allergic or hypersensitive to any constituents of Ganoderma lucidum or any member of its family. Use cautiously with diabetes, blood disorders (including hemophilia), low blood pressure, or ulcers. Avoid if pregnant or breastfeeding.
Rhubarb: Two studies have been conducted on rhubarb and its effects on hepatitis. In the case series, high doses of rhubarb decreased the symptoms and serum levels associated with hepatitis. However, additional, high-quality studies are needed to establish rhubarb's effects.
Avoid if allergic/hypersensitive to rhubarb, its constituents, or related plants from the Polygonaceae family. Avoid using rhubarb for more than two weeks because it may induce tolerance in the colon, melanosis coli, laxative dependence, pathological alterations to the colonic smooth muscles, and substantial loss of electrolytes. Avoid with atony, colitis, Crohn's disease, dehydration with electrolyte depletion, diarrhea, hemorrhoids, insufficient liver function, intestinal obstruction or ileus, irritable bowel syndrome, menstruation, pre-eclampsia, renal disorders, ulcerative colitis, and urinary problems. Avoid handling rhubarb leaves, as they may cause contact dermatitis. Avoid rhubarb in children under age 12 due to water depletion. Use cautiously with bleeding disorders, cardiac conditions, coagulation therapy, constipation, history of kidney stones, or thin or brittle bones. Use cautiously if taking anti-psychotic drugs or oral drugs, herbs or supplements (including calcium, iron, and zinc). Avoid if pregnant or breastfeeding.
Safflower: EH0202 is a traditional Japanese Kampo therapy containing safflower seed extract and is used for immunostimulation. More studies with safflower alone are needed to better define safflower's effect on chronic hepatitis.
Avoid if allergic/hypersensitive to safflower, Carthamus tinctorius, safflower oil, daisies, ragweed, chrysanthemums, marigolds, or any related constituents. Use parenteral safflower oil emulsions cautiously in newborns. Use cautiously if taking anticoagulants (blood thinners) or anti-platelet drugs, immunodepressants, or pentobarbital. Use cautiously with diabetes, hypotension, inadequate liver function, hypercoagulability, and skin pigmentation conditions. Use cautiously if pregnant or breastfeeding.
SAMe: Preliminary evidence from meta-analyses and randomized clinical trials suggests that SAMe may normalize levels of liver enzymes in individuals with liver disease. Well-designed clinical trials, with appropriate subject number in homogenous populations are required before a definitive conclusion can be made.
Avoid if allergic or hypersensitive to SAMe. Use cautiously with diabetes and anxiety disorders, or women in their third trimester of pregnancy. Avoid with bipolar disorder. Avoid during the first trimester of pregnancy or if breastfeeding.
Schisandra: The efficacy of schisandra as a hepatoprotective agent has been demonstrated in multiple studies. Based on these observations, schisandra has been suggested as a potential treatment for liver disease. Future studies are warranted to assess the long-term efficacy and safety of schisandra compared to standard therapies.
Use cautiously during pregnancy or lactation or in patients with bleeding disorders, seizure disorders, high intracranial pressure, high blood pressure, skin diseases, gastoeseophageal reflux or peptic ulcer disease, neurological disorders, or diabetes. Avoid in patients allergic to schisandra, any of its constituents, or other members of the Schisandraceae family. Allergic skin rashes and urticaria has been reported in some patients.
Sea buckthorn: Sea buckthorn extract may improve liver health in people with cirrhosis. Although the results are intriguing, additional higher quality research is needed in this area.
Avoid if allergic or hypersensitive to sea buckthorn, its constituents, or members of the Elaeagnaceae family. Use cautiously if taking angiotensin converting enzyme (ACE) inhibitors, anticoagulants and antiplatelet agents (blood thinners), antineoplastics (anticancer agents), or cyclophosphamide or farmorubicin. Avoid higher doses than food amounts if pregnant or breastfeeding.
Selenium: Selenium supplementation has been studied in various liver disorders, including hepatitis, with mixed results. Further research is needed to establish selenium's effects on liver disease.
Avoid if allergic or sensitive to products containing selenium. Long-term ingestion of excessive doses may cause toxicity to skin, nails, bones, teeth, and possibly the central nervous system. Avoid with history of nonmelanoma skin cancer. Selenium is generally regarded as safe for pregnant or breastfeeding women. However, animal research reports that large doses of selenium may lead to birth defects.
Taurine: Early studies have found that taurine supplementation has the potential to modify the conjugation of bile acids, potentially modifying the disease. Furthermore, taurine has been examined as an adjunct to ursodeoxycholate (UDCA) in the treatment of liver disease. Results from these early studies suggest that conjugation of bile acids can be modified and that taurine as an adjunct to UDCA does not offer more benefits. More recent studies are investigating the effect of tauroursodeoxycholate (TUDCA) in liver disease treatment. As of yet, however, the evidence in support of taurine in liver disease is minimal and well-designed clinical trials with positive results are needed before a firm conclusion can be made.
Taurine is an amino acid and it is unlikely that there are allergies related to this constituent. However, allergies may occur from multi-ingredient products that contain taurine. Use cautiously in patients with high cholesterol, low blood pressure, coagulation disorders, potential for mania, or epilepsy. Avoid consuming alcohol or exercising after consumption of energy drinks containing taurine, caffeine, glucuronolactone, B vitamins, and other ingredients. Use cautiously if pregnant or breastfeeding because taurine is a natural component of breast milk.
Thymus extract: Preliminary evidence suggests that thymus extract may offer benefit to individuals with liver disease. More well-designed clinical trials are required.
Avoid if allergic or hypersensitive to thymus extracts. Use bovine thymus extract supplements cautiously due to potential for exposure to the virus that causes "mad cow disease." Avoid use with an organ transplant or other forms of allografts or xenografts. Avoid if receiving immunosuppressive therapy, with thymic tumors, myasthenia gravis (neuromuscular disorder), untreated hypothyroidism, or if taking hormonal therapy. Avoid if pregnant or breastfeeding; thymic extract increases human sperm motility and progression.
Traditional Chinese medicine (TCM): Traditional Chinese medicine (TCM) may provide protection for liver disease. However, more studies are needed before recommendations can be made.
Chinese herbs can be potent and may interact with other herbs, foods, or drugs. A qualified healthcare professional should be consulted before taking. There have been reports of manufactured or processed Chinese herbal products being tainted with toxins or heavy metal or not containing the listed ingredients. Herbal products should be purchased from reliable sources.
Turmeric: In traditional Indian Ayurvedic medicine, turmeric has been used to tone the liver. Early research suggests that turmeric may have a protective effect on the liver. More research is needed to better determine the effectiveness of turmeric for liver protection.
Avoid if allergic or hypersensitive to turmeric, curcumin, yellow food colorings, or plants belonging to the Zingiberaceae (ginger) family. Use cautiously with a history of bleeding disorders, immune system deficiencies, liver disease, diabetes, hypoglycemia, or gallstones. Use cautiously with blood-thinners, such as warfarin (like Coumadin®), and blood sugar-altering medications. Avoid in medicinal amounts if pregnant or breastfeeding. Turmeric should be stopped prior to scheduled surgery.
Vitamin A: There is insufficient evidence to support or refute the benefits or adverse effects of antioxidant supplements, such as vitamin A, in patients with liver disease.
Vitamin A toxicity can occur if taken at high dosages. Vitamin A appears to be safe in pregnant women if taken at recommended doses. However, vitamin A excess, as well as deficiency, has been associated with birth defects. Vitamin A is excreted in human breast milk. The benefits or dangers to nursing infants are not clearly established. Use cautiously in children and infants. Use cautiously in patients using alcohol, bile acid sequestrants, birth control pills, chemotherapeutic agents (such as busulfan), mineral oil, neomycin, or orlistat. Avoid if allergic or hypersensitive to vitamin A. Avoid with agents toxic to the liver, blood thinners (such as warfarin (Coumadin®)), retinoids, or tetracycline antibiotics. Avoid in patients with liver disease, intestinal infections, fat malabsorption syndromes, severe protein energy malnutrition, or type V hyperlipoproteinemia (a genetic disorder). Avoid high-dose vitamin A and beta-carotene in patients at high risk of lung cancer.
Vitamin C: Administration of vitamin C in individuals with cirrhosis may have some benefit. However, in patients with chronic hepatitis C, vitamin C was not effective. Additional studies are needed before a conclusion can be made on the use of vitamin C in patients with liver disease.
Vitamin C is generally considered safe in amounts normally found in foods. Vitamin C supplements are also generally considered safe in most individuals if taken in recommended doses. Vitamin C intake from food is generally considered safe if pregnant or breastfeeding. It is not clear if vitamin C supplements in doses higher than Dietary Reference Intake recommendations are safe for pregnant or breastfeeding women. Vitamin C is naturally found in breast milk. High doses of vitamin C have been associated with multiple adverse effects. In postmenopausal women with diabetes, daily vitamin C in doses greater than 300 milligrams has been linked to heart-related death. Vitamin C in high doses appears to interfere with the blood-thinning effects of anticoagulants such as warfarin by lowering prothrombin time (PT). Therefore, caution is advised in patients with bleeding disorders or those taking drugs that affect bleeding. Vitamin C may affect blood sugar levels. Therefore, caution is advised in patients with diabetes or hypoglycemia, and in those taking drugs, herbs, or supplements that affect blood sugar. Use with caution in patients with cancer, glucose-6-phosphate dehydrogenase deficiency, anemia and related conditions, kidney stones, or sickle cell disease, or after angioplasty. Use with caution in patients taking antibiotics, anticancer agents, HIV medications, barbiturates, estrogens, fluphenazine, or iron supplements. Use parenteral (injected) vitamin C cautiously. Avoid in patients with known allergy or sensitivity to any vitamin C product ingredients. Avoid high doses of vitamin C in patients with cirrhosis, gout, renal tubular acidosis, paroxysmal nocturnal hemoglobinuria, or kidney failure, or in those taking agents that may damage the kidneys.
Vitamin E: In patients with hepatitis on antiviral therapy, vitamin E has been proposed to prevent inflammation. More studies are needed. There is also preliminary evidence suggesting possible benefits of vitamin E in the management of fatty liver disease in children, although further evidence is necessary before a clear conclusion can be drawn.
Avoid if allergic or hypersensitive to vitamin E. Avoid with retinitis pigmentosa (loss of peripheral vision). Use cautiously with bleeding disorders or if taking blood thinners. Avoid above the recommended daily level in pregnant and breastfeeding women.
Whey protein: Although not well studied in humans, whey protein may have liver protective effects. High quality clinical studies are needed to make a conclusion on the use if whey protein in patients with hepatitis.
Use with caution when taken in combination with any other drugs, herbs, or supplements. Use with caution in people with diabetes, low blood sugar, low blood pressure, bleeding disorders, gastrointestinal disorders, in those taking agents to treat any of these conditions, or in those taking agents which lower cholesterol, affect the immune system, or are broken down by the liver. Use caution while operating heavy machinery. Avoid the use of excessive doses for long periods of time, and of non-approved sources in infant formula. Avoid use if pregnant or breastfeeding, in people with known allergy or sensitivity to milk or milk products, and in those avoiding dairy products.
Zinc: Zinc is necessary for the functioning of over 300 different enzymes and plays a vital role in an enormous number of biological processes. People with alcoholic liver cirrhosis may be deficient in zinc. Preliminary studies suggest that zinc may benefit these patients. Further evidence is needed to confirm these findings. Studies have shown that zinc, in combination with interferon or interferon and ribavirin for chronic hepatitis C viral infection, did not show significant benefits except for lower incidence of gastrointestinal side effects. Further study may be warranted. Early human trials of zinc for hepatic encephalopathy have yielded conflicting results.
Zinc is generally considered safe when taken at the recommended dosages. Avoid zinc chloride since studies have not been done on its safety or effectiveness. While zinc appears safe during pregnancy in amounts lower than the established upper intake level, caution should be used since studies cannot rule out the possibility of harm to the fetus.
Fair negative scientific evidence:
N-acetyl cysteine: There is fairly strong evidence that NAC does not increase a hepatitis patient's response to interferon therapy. Additional research is needed.
Use with caution in patients with bleeding disorders or taking drugs that may increase the risk of bleeding, in patients with blood pressure disorders or taking agents that affect blood pressure, or in patients with diabetes, high or low blood sugar, or taking agents that affect blood sugar. Use with caution in patients with heart disease, gastrointestinal disorders, breathing disorders, zinc deficiency, unpleasant mood, or those complaining of dizziness, lightheadedness, or visual complaints. Use with caution in those using antibiotics, nitroglycerin, or needing charcoal treatment. Avoid in doses greater than 30 grams daily. Avoid in pregnant or breastfeeding women. Avoid with known allergy or sensitivity to NAC or related substances.
Spirulina: Despite findings indicating potential hepatoprotective properties of spirulina, preliminary human study of spirulina for chronic viral hepatitis shows negative results. Additional high quality study is needed to confirm these findings.
Avoid if allergic or hypersensitive to spirulina or blue-green algae. Use cautiously with phenylketonuria (a genetic disorder of a liver enzyme that disrupts normal body functions), autoimmune diseases, bleeding disorders, diabetes, and osteoporosis. Use cautiously with products containing the blue-green algae species Anabaena spp., Aphanizomenon spp., and Microcystis spp.; in underweight patients or in those taking antiobesity agents or appetite suppressants; and if consuming a high-protein diet. Avoid in children and if pregnant or breastfeeding.
Urine therapy: There is currently insufficient evidence from clinical studies to support the use of urine or urea in the treatment of liver cancer. Additional studies are needed to make a firm recommendation.
Use cautiously in children, if taking medications, especially antidepressants, antipsychotics and/or sedative/hypnotic agents, or with gastrointestinal problems. Avoid with urinary tract or kidney infection or if pregnant or breastfeeding. Avoid if allergic or hypersensitive to urine or any of its metabolites.
Prevention
Reducing alcohol and drug consumption: Drink alcohol in moderation, if at all. Over many years, more than one drink a day for women and more than two drinks a day for men may be enough to lead to cirrhosis. Use of certain drugs, including some illegal drugs (such as cocaine, heroin, and methamphetamine), may also cause liver disease. If fatty liver or hepatitis exists, no alcohol should be consumed.
Only use prescription and nonprescription drugs when needed and take only the recommended doses. Acetaminophen (Tylenol®) dosages should be followed specifically as stated by the manufacturer or by a healthcare provider. The manufacturer has set a maximum dose of 4 grams of acetaminophen (the equivalent of eight extra-strength tablets or capsules, 500 milligrams each) per day. However, healthcare professionals recommend that individuals who take prescription medications or drink alcohol daily should only take a maximum of 2-3 grams per 24 hours. Many over-the-counter (OTC) products may also contain acetaminophen (Tylenol®). It is important not to exceed the total daily dosage of four grams acetaminophen. Acetaminophen should only be used for the short-term (no more than two weeks) treatment of conditions such as minor aches and pains. Particular caution is need in dosing infants with acetaminophen to ensure that the correct dose is given.
Do not mix other drugs with alcohol. Acetaminophen (Tylenol®) can be toxic to the liver even if individuals drink in moderation.
Hepatitisvaccination: If an individual is at increased risk of contracting hepatitis or if they already been infected with any form of the hepatitis virus, a doctor will recommend the hepatitis B vaccine. A vaccine is also available for hepatitis A.
Dietary supplements: Herbal supplements that can be toxic to the liver may include kava kava (Piper methysticum), chaparral (Larrea taridentata), comfrey (Symphytum officinale), germander (Teucrium chamaedrys), kombucha tea, mistletoe (Viscum album), pennyroyal (Mentha pulegium), and skullcap (Scutellaria laterifolia). Also, avoid high doses of fat soluble vitamins, including vitamins A, D, E, and K, as they can also be potentially toxic to the liver.
Avoiding contact with blood and body fluids from others: Hepatitis viruses can be spread by accidental needle sticks, improper cleanup of blood or body fluids, and sharing intravenous needles. It is also possible to become infected by sharing razor blades or toothbrushes or by having unsafe sex.
Avoiding chemical toxins: When using toxic chemicals such as cleaners, ventilating the room or wearing a mask is important. Take similar protective measures when spraying insecticides, fungicides, paint, and other toxic chemicals. When using insecticides and other toxic chemicals, covering the skin with gloves, long sleeves, a hat, and a mask is recommended by healthcare professionals. Chemical toxins may damage liver cells and cause liver dysfunction.
Weight control: Maintaining proper weight through diet and exercise is important. Even if an individual does not drink alcohol, obesity can cause nonalcoholic fatty liver disease, which may include fatty liver, hepatitis, and cirrhosis.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
American Liver Foundation. www.liverfoundation.org.
American Gastroenterological Association. www.gastro.org.
Centers for Disease Control and Prevention. www.cdc.gov.
De Piano A, Prado WL, Caranti DA, et al. Metabolic and nutritional profile of obese adolescents with nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr. 2007;44(4):446-52. View Abstract
Hepatitis Foundation International. www.hepfi.org.
Khanna S, Gopalan S. Role of branched-chain amino acids in liver disease: the evidence for and against. Curr Opin Clin Nutr Metab Care. 2007;10(3):297-303. View Abstract
Maher JJ. Alcoholic steatohepatitis: management and prognosis. Curr Gastroenterol Rep. 2007;9(1):39-46. View Abstract
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Peng S, Plank LD, McCall JL, et al. Body composition, muscle function, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr. 2007;85(5):1257-66. View Abstract
Sargent S. Pathophysiology and management of hepatic encephalopathy. Br J Nurs. 2007;16(6):335-9. View Abstract
Yamamoto M, Iwasa M, Iwata K, et al. Restriction of dietary calories, fat and iron improves non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2007;22(4):498-503. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017