Head Injury
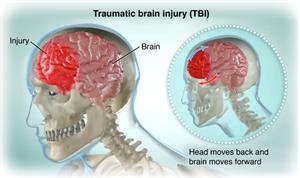
A head injury is a broad term that describes a vast array of injuries that occur to the scalp, skull, brain, and underlying tissue and blood vessels in the head. Head injuries are also commonly referred to as brain injury, or traumatic brain injury (TBI), depending on the extent of the head trauma.
Head injuries are one of the most common causes of disability and death in adults. The injury can be as mild as a bump, bruise (contusion), or cut on the head, or can be moderate to severe in nature due to a concussion, deep cut or open wound, fractured skull bone(s), or from internal bleeding and damage to the brain.
These are some of the different types of head injuries:
- Concussion. A concussion is an injury to the head area that may cause instant loss of awareness or alertness for a few minutes up to a few hours after the traumatic event.
- Skull fracture. A skull fracture is a break in the skull bone. There are 4 major types of skull fractures, including the following:
- Linear skull fractures. This is the most common type of skull fracture. In a linear fracture, there is a break in the bone, but it does not move the bone. For this type of fracture, your doctor may observe you in the hospital for a brief time. Usually, you will not need treatment and you can resume normal activities in a few days.
- Depressed skull fractures. You may or may not have a cut in the scalp with this type of fracture. In this fracture, part of the skull is actually sunken in from the trauma. This type of skull fracture may require surgery, depending on the severity, to help correct the deformity.
- Diastatic skull fractures. These fractures occur along the suture lines in the skull. The sutures are the areas between the bones in the head that fuse during childhood. In this type of fracture, the normal suture lines are widened. Newborns and older infants are more likely to get these types of fractures.
- Basilar skull fracture. This is the most serious type of skull fracture, and involves a break in the bone at the base of the skull. With this type of fracture, you may have bruises around the eyes and a bruise behind the ear. You may also have clear fluid draining from the nose or ears due to a tear in part of the covering of the brain. If you have this type of fracture, you will require close observation in the hospital.
- Intracranial hematoma (ICH). An intracranial hematoma is a blood clot in or around the brain. There are different types of hematomas, classified by their location in the brain. These can cause mild head injuries to quite serious and potentially life-threatening injuries. The different types of intracranial hematomas include:
- Epidural hematoma. Epidural hematomas occur when a blood clot forms underneath the skull, but on top of the tough covering that surrounds the brain (the dura). They usually come from a tear in an artery that runs just under the skull. Epidural hematomas are usually associated with a skull fracture.
- Subdural hematoma. Subdural hematomas occur when a blood clot forms underneath the skull and underneath the dura, but outside of the brain. These can form from a tear in the veins that go from the brain to the dura, or from a cut on the brain itself. They are sometimes, but not always, associated with a skull fracture.
- Contusion or intracerebral hematoma. A contusion is a bruise to the brain itself. A contusion causes bleeding and swelling inside of the brain around the area where the head was struck. Contusions may occur along with a fracture or other blood clots. Bleeding that occurs inside the brain itself can sometimes occur spontaneously. When trauma is not the cause, the most common causes are long-standing high blood pressure in older adults, bleeding disorders in either children or adults, or the use of medicines that cause blood thinning, or certain illicit drugs.
- Diffuse axonal injury (DAI). These injuries are common and are usually caused by shaking of the brain back and forth, which can happen in car accidents, from falls, or shaken baby syndrome. Diffuse injuries can be mild, such as with a concussion, or may be very severe, as in diffuse axonal injury. If severe, you may be in a coma for a prolonged period, with injury to many different parts of the brain.
There are many causes of head injury in children and adults. The most common traumatic injuries are from motor vehicle accidents (automobiles, motorcycles, or struck as a pedestrian), from violence, from falls, or from child abuse. Subdural hematomas and brain hemorrhages can sometimes happen spontaneously.
When there is a direct blow to the head, shaking of the child, or when a whiplash-type injury occurs, the brain jolts backwards and hits the skull on the opposite side, causing a bruise. The jarring of the brain against the sides of the skull can cause tearing of the internal lining, tissues, and blood vessels that may cause internal bleeding, bruising, or swelling of the brain.
Young children, older adults and males are at most risk for head injuries. Those who don’t use child car seats, seat belts, or safety helmets are also at increased risk for head injuries.
Symptoms vary depending on the severity of the head injury. These are the most common symptoms of a head injury.
Mild head injury
Symptoms include:
- Raised, swollen area from a bump or a bruise
- Small, superficial (shallow) cut in the scalp
- Headache
- Sensitivity to noise and light
- Irritability
- Confusion
- Lightheadedness or dizziness
- Problems with balance
- Nausea
- Problems with memory or concentration
- Change in sleep patterns
- Blurred vision
- "Tired" eyes
- Ringing in the ears (tinnitus)
- Alteration in taste
- Fatigue or lethargy
Moderate to severe head injury
This requires immediate medical attention. Symptoms may include any of the above plus:
- Loss of consciousness
- Severe headache that does not go away
- Repeated nausea and vomiting
- Loss of short-term memory, such as difficulty remembering the events that led right up to and through the traumatic event
- Slurred speech
- Trouble walking
- Weakness in one side or area of the body
- Sweating
- Pale skin color
- Seizures or convulsions
- Behavior changes including irritability
- Blood or clear fluid draining from the ears or nose
- One pupil (dark area in the center of the eye) is dilated, or looks larger, than the other eye and doesn't constrict, or get smaller, when exposed to light
- Deep cut or laceration in the scalp
- Open wound in the head
- Foreign object penetrating the head
- Coma (when you are unconscious and can’t be awakened, don’t respond to stimuli)
- Vegetative state (when you have lost thinking abilities and awareness of your surroundings, but can do basic functions such as breathing and blood circulation)
- Locked-in syndrome (a neurological condition in which a person is conscious and can think and reason, but can’t speak or move)
The symptoms of a head injury may look like other problems or medical conditions. Always see your healthcare provider for a diagnosis.
The full extent of the head injury may not be completely understood immediately after the injury. You will need comprehensive evaluation and testing. A physical exam and other tests help make the diagnosis of a head injury. During the exam, the healthcare provider will ask about your medical history and how you were injured. Trauma to the head can cause neurological problems and may require further medical follow up.
Diagnostic tests may include:
- Blood tests
- X-ray. This test that uses electromagnetic energy beams to make images of internal tissues, bones, and organs onto film.
- Computed tomography scan (also called a CT or CAT scan). This procedure uses a combination of X-rays and computer technology to make images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
- Electroencephalogram (EEG). This procedure records the brain's continuous, electrical activity by means of electrodes attached to the scalp.
- Magnetic resonance imaging (MRI). This test uses large magnets, radiofrequency energy, and a computer to make detailed images of organs and structures in the body.
Your healthcare provider will determine the best treatment based on:
- How old you are
- Your overall health and medical history
- How sick you are
- How well you can handle specific medicines, procedures, or therapies
- How long the condition is expected to last
- Your opinion or preference
For a severe head injury, you are monitored for increased intracranial pressure (pressure inside the skull). Head injury may cause the brain to swell. Since the brain is covered by the skull, there is only a small amount of room for it to swell. This causes pressure inside the skull to increase, which can lead to brain damage.
Intracranial pressure is measured in one of two ways.- One way is to place a small hollow tube (catheter) into the fluid-filled space in the brain (ventricle).
- The second way is to use a small, hollow device (bolt) placed through the skull into the space just between the skull and the brain.
A head injury can result in loss of muscle strength, fine motor skills, speech, vision, hearing, or taste function, depending on the brain region involved and the severity of brain damage. Long- or short-term changes in personality or behavior may also occur. You may need long-term medical and rehabilitative (physical, occupational, or speech therapy) management.
The key to head injury prevention is to promote a safe environment for children and adults and to prevent head injuries from occurring in the first place. The following measures can help prevent head injury:
- Use car seats and seat belts when riding in the car and helmets (when worn properly) for activities, such as bicycle riding, in-line skating, skiing, and skateboarding.
- Prevent falls. Since older adults are prone to falls, it is important to make their living areas safe by removing throw rugs or clutter that may cause them to trip, installing handrails in the bathroom and stairways, and assuring that there is good lighting.
- For young children, it is important to secure windows with window guards and safety gates.
Seek immediate medical attention if any of these occur:
- A laceration (cut)
- Persistent or increasing sleepiness or confusion
- Seizure, repeated vomiting, or severe headache
- Inability to feel an arm or leg or recognize people
- Loss of balance
- Difficulty speaking, seeing, or breathing
- Loss of consciousness
- A head injury is a broad term that describes a vast array of injuries that occur to the scalp, skull, brain, and underlying tissue and blood vessels in the head.
- The most common traumatic injuries are from motor vehicle accidents from violence, from falls, or from child abuse.
- Moderate to severe head injury requires immediate medical attention.
- Severe head injury requires close monitoring for increased intracranial pressure.
- Prevention is most important by promoting a safe environment for children and adults through the use of car seats, seat belts, and helmets, and removing tripping and fall hazards in the home.
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
January 16, 2018
Sources:
Traumatic brain injury: Epidemiology, classification, and pathophysiology, Up To Date
Reviewed By:
Shelat, Amit, MD,Dozier, Tennille, RN, BSN, RDMS