Alstrom syndrome
Alstrom syndrome
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
ALMS, ALMS1 human, ALSS, Alström-Hallgren syndrome, blindness, cardiomyopathy, deafness, KIAA0328.
Background
Alström syndrome is a rare, progressive genetic disorder, with characteristic deafness, obesity, and visual problems in children, and diabetes with insulin resistance (type 2) and kidney failure in adults. In infancy, the earliest signs are usually extreme photophobia (light sensitivity) and nystagmus (a back-and-forth movement of the eyes). Another early sign may be dilated cardiomyopathy (an enlarged heart) and congestive heart failure in infants less than one year of age. For the first year of life, infants with Alström syndrome gain excessive weight, leading to obesity. Numerous organ systems may be affected later, resulting in blindness, hearing impairment, heart failure, diabetes mellitus type 2, liver disease, pulmonary fibrosis, renal (kidney) failure, and urological dysfunction.
Alström syndrome is caused by mutations or defects in the Alström syndrome 1 or ALMS1 gene, which provides instructions for making a protein with a currently unknown function. Researchers believe that the protein may play a role in hearing, vision, regulation of body weight, and functions of the heart, kidney, lungs, and liver. It may also affect how the pancreas regulates insulin, a hormone that helps control blood sugar levels. More than 80 mutations in the ALMS1 gene have been identified in people with Alström syndrome. Most of these mutations lead to the production of a dysfunctional version of the ALMS1 protein.
Alström syndrome is inherited, or passed down among family members, as an autosomal recessive trait. This means that two copies of the causative gene must be inherited for the disease to occur.
Alström syndrome is extremely rare, with only about 425 cases recorded worldwide. Its exact prevalence is unknown, but the syndrome is more common among people of French-Acadian heritage.
Risk Factors
Alström syndrome is inherited, or passed down among family members. Therefore, the only known risk factor is a family history of the disorder. Although the exact prevalence is unknown, the incidence of Alström syndrome appears to be higher among people of French-Acadian heritage. If one parent is a carrier, or has only one copy of the defective gene, then each child has a 50% chance of inheriting one defective gene and also being a carrier. If both parents are carriers, each child has a 25% chance of inheriting two defective genes, a 50% chance of inheriting only one defective gene, and a 25% chance of inheriting neither defective gene. Alström syndrome appears to affect males and females equally.
Causes
Genetic mutations: Alström syndrome is caused by mutations or defects in the Alström syndrome 1 or ALMS1 gene, which encodes for a protein with a currently unknown function. Researchers believe the protein may play a role in normal hearing, sight, weight regulation, and functioning of the heart, kidney, lungs, liver, and pancreas. This protein is present in virtually all tissues of the body, which may explain why nearly every system in the body is affected by Alström syndrome.
Autosomal recessive inheritance: Alström syndrome follows an autosomal recessive pattern of inheritance, meaning that an individual must inherit two copies of the defective gene, one from each parent. Individuals who inherit only one copy of the defective ALMS1 gene generally have no symptoms and are called carriers, because they can pass on the disorder to their children.
If one parent is a carrier, or has only one copy of the defective gene, then each child has a 50% chance of inheriting one defective gene and also being a carrier. If both parents are carriers, each child has a 25% chance of inheriting two defective genes, a 50% chance of inheriting only one defective gene, and a 25% chance of inheriting neither defective gene. Therefore, if both parents are carriers, about one out of four children will have Alström syndrome.
Random occurrence: It not known whether Alström syndrome occurs as the result of a spontaneous mutation in the egg, sperm cells, or developing embryo.
Signs and Symptoms
General: Signs and symptoms of Alström syndrome tend to appear in infancy or early childhood. Symptoms of the disorder may vary widely, even among members of the same family.
Developmental delay: About 20% of affected individuals have delays in early developmental milestones, including delays in gross and fine motor skills and in expressive and receptive language, and about 30% have a learning disability. Severe intellectual disability, characterized by an intelligence quotient (IQ) under 70, is very rare.
Diabetes: People with Alström syndrome are prone to developing type 2 diabetes early in life. Diabetes, also known as diabetes mellitus, is a chronic health condition in which the body is unable to produce enough insulin and properly break down glucose (sugar) in the blood. Symptoms of diabetes include frequent urination, excessive thirst, extreme hunger, unusual weight loss, increased fatigue, irritability, and blurry vision.
Hearing: Up to 70% of people with Alström syndrome gradually lose hearing during the first decade of life. By age 20, hearing loss may be classified as severe or moderately severe. People with Alström syndrome may also be prone to developing "glue ear," in which a sticky substance collects in the ear canal, further obstructing hearing.
Heart: Individuals with Alström syndrome may develop a condition called cardiomyopathy, in which the muscular walls of the heart weaken. In dilated cardiomyopathy, the heart is not able to pump blood efficiently. Symptoms may include irregular heartbeat, fatigue, and shortness of breath. About 40% of people with Alström syndrome develop cardiomyopathy between the ages of three weeks and four months. Most of these children make a full recovery in infancy and survive into adulthood. More than 60% of people with Alström syndrome develop heart failure at some stage in their lives.
High cholesterol: People with Alström syndrome may have high levels of triglycerides and total cholesterol in the blood. Very high levels of triglycerides have been associated with pancreatitis (inflammation of the pancreas) in individuals with Alström syndrome.
Kidney disease: Kidney disease is typically recognized later in life in individuals with Alström syndrome. Signs of kidney disease include frequent urination and extreme thirst. End-stage kidney disease may occur as early as the teenage years.
Lungs: Individuals with Alström syndrome may develop lung problems, which may include susceptibility to bronchitis and pulmonary hypertension (high blood pressure that affects the arteries in the lungs).
Obesity: Although people with Alström syndrome generally are of normal weight at birth, they may become obese during childhood. In particular, people with Alström syndrome gain fat in the abdominal area. In adults, obesity is defined as a body-mass index (BMI) of 30 or greater. In some individuals with Alström syndrome, weight may be in the high normal range after adolescence. Some researchers believe that a mutation in the ALMS1 gene may lead to these weight changes.
Skeletal abnormalities: Almost all people with Alström syndrome are of short stature. Other skeletal abnormalities may include scoliosis (sideways curvature of the spine) or kyphosis (forward curvature of the spine), especially during puberty.
Skin: Some individuals with Alström syndrome develop a skin condition called acanthosis nigricans. In this condition, the skin folds in the underarms or on the neck become thickened, dark, and velvety. This condition is often associated with diabetes.
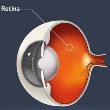
Vision: Normal vision is gradually lost in almost all patients with Alström syndrome. This is caused by cone-rod dystrophy, sensitivity to light, and nystagmus (involuntary movements of the eyes). Vision loss usually begins at around age 15 months. By 20 years of age, individuals with Alström syndrome typically cannot perceive light. People with Alström syndrome may often touch, press, or rub their eyes.
Other: Liver problems may be present in people with Alström syndrome. Underactive thyroid and underdeveloped male genitals may also be observed in Alström syndrome. While some individuals with Alström syndrome may have growth and developmental delays, intelligence is usually not affected. About 30% of people with Alström syndrome have a learning disability.
Diagnosis
General: A thorough physical exam and family history should be completed if Alström syndrome is suspected. The diagnosis of Alström syndrome is based on characteristic clinical features that emerge throughout infancy, childhood, and young adulthood. In particular, obesity occurs in early childhood, hearing impairments usually develop between ages one and 10 years, and childhood or adolescent cardiomyopathy occurs in more than 60% of affected individuals. Development of diabetes, liver disease, and progressive kidney disease; and developmental delay of fine and gross motor skills and receptive or expressive language skills have been described in some individuals, and some school-age children experience academic difficulties.
Fasting blood glucose test: Fasting blood glucose testing checks blood glucose levels after fasting for 12-14 hours. The individual may drink water during this time but should strictly avoid any other beverage. Individuals with diabetes may be asked to delay their diabetes medication or insulin dose until the test is completed. This test can be used to diagnose diabetes or prediabetes. The fasting plasma glucose (FPG) test is preferred for diagnosing diabetes, because it is convenient and reliable when done on an empty stomach in the morning. When done at other times of day, the presence of food and natural biorhythms may cause fluctuations in blood sugar levels and an inaccurate test result.
If the fasting glucose level is 100-125 milligrams per deciliter, the individual has a form of prediabetes called impaired fasting glucose (IFG), meaning that the he or she is more likely to develop type 2 diabetes than with a lower glucose level but does not yet have the condition. A level of 126 milligrams per deciliter or higher, confirmed by testing on another day, means that the individual has diabetes.
Oral glucose tolerance test: During an oral glucose tolerance test (OGTT), a high-glucose drink is given to the individual to determine how quickly the glucose is cleared from the blood. High glucose levels, meaning that the glucose was not normally cleared from the blood, may indicate diabetes. Blood samples are checked at regular intervals for two hours. Glucose tolerance tests are used when the results of the fasting blood glucose test are inconclusive. They are also used to diagnose gestational diabetes (diabetes in pregnancy). This test can be used to diagnose diabetes or prediabetes.
Blood tests: A sample of blood may be taken to measure liver, kidney, and thyroid function. The blood urea nitrogen (BUN) test evaluates kidney function in individuals with Alström syndrome. Urea is a by-product of protein metabolism. This waste product is formed in the liver, then filtered from the blood and excreted in the urine by the kidneys. The BUN test measures the amount of nitrogen present in the urea. High BUN levels may indicate kidney dysfunction, but BUN may also be affected by protein intake and liver function. A blood creatinine test is also performed. This test measures blood levels of creatinine, a by-product of energy metabolism that, like urea, is filtered from the blood by the kidneys and excreted into the urine. An individual's muscle mass determines the amount of creatinine produced. With normal kidney function, the amount of creatinine in the blood remains relatively constant, since muscle mass usually fluctuates very little. Due to this consistency, and because creatinine is affected very little by liver function, a blood creatinine level is a more sensitive indicator of kidney function than BUN. Liver function tests (LFTs) are a set of blood tests that may help determine how well an individual's liver is working. LFTs measure albumin, bilirubin, cholesterol, liver enzymes (ALT, AST, GGT, and ALP), prothrombin time, and total protein. The blood levels of thyroid hormones can be measured directly to detect thyroid hormone functioning.
Eye exam: A thorough eye exam may identify nystagmus (involuntary movements of the eyes), sensitivity to light, and poor color perception. These problems are often detectable during the first year of life.
Hearing test: A hearing test, called an audiogram, may help diagnose Alström syndrome. During an audiogram, the patient is exposed to various sounds of different pitches and frequencies through headphones. The patient is asked to identify each time a sound is heard. The audiologist may also say various words to evaluate the patient's hearing ability. Hearing loss in Alström syndrome may progress to the severe or moderately severe range (40-70 decibels) between the ages of 10 and 20 years old.
Hemoglobin A1c: The hemoglobin A1c test is an advantageous measure of blood glucose control over an extended period of time. The American Diabetes Association currently recommends an A1c goal of less than 7.0%, which corresponds to a mean blood glucose level of 170 milligrams per deciliter. Since individuals with Alström syndrome may not effectively clear glucose from the blood, it is likely that their A1c percentages would be high.
Imaging studies: An electroretinography (ERG) can establish the presence of cone-rod dystrophy, a progressive disease that causes the breakdown of the rods and cones in the retina and usually results in blindness. An electrode is placed behind the lower eyelid, allowing it to touch the cornea, or the clear layer on the outside of the eye, and another is placed on the skin near the eye. During a recording, the patient's eyes are exposed to various stimuli and the response signal is recorded.
Other imaging studies such as X-rays may be used to diagnose and track progress of scoliosis (sideways curvature of the spine) or kyphosis (forward curvature of the spine). An echocardiogram (ECG) is an ultrasound of the heart muscle from which a clinician can determine aspects of the structure and function of the heart. A chest X-ray may reveal lung problems, such as chronic bronchitis, frequent pneumonia, chronic obstructive pulmonary disease (COPD), and pulmonary hypertension (high blood pressure within the artery in the lung).
Genetic testing: If Alström syndrome is suspected, a cytogenetic test may be performed to confirm a diagnosis. A sample of the patient's blood is taken and analyzed in a laboratory for a defect in the ALMS1 gene. If this defect is detected, a positive diagnosis is made.
Prenatal DNA testing: If there is a family history of Alström syndrome, prenatal testing may be performed to determine whether the fetus has the disorder. Amniocentesis and chorionic villus sampling (CVS) can diagnose Alström syndrome. However, because there are serious risks associated with these tests, patients should discuss the potential health benefits and risks associated with these procedures with a medical professional.
During amniocentesis, a long, thin needle is inserted through the abdominal wall and into the uterus, and a small amount of amniotic fluid is removed from the sac surrounding the fetus. Cells in the fluid are then analyzed for normal and abnormal chromosomes. This test is performed after 15 weeks of pregnancy. The risk of miscarriage is about one in 200-400 patients. Some patients may experience minor complications, such as cramping, leaking fluid, or irritation where the needle was inserted.
Chorionic villus sampling (CVS), requires removal of a small piece of tissue (chorionic villi) from the placenta between the ninth and 14th weeks of pregnancy. CVS may be performed through the cervix or through the abdomen. The cells in the tissue sample are then analyzed for the mutation in the ALMS1 gene. The risk of miscarriage is about 0.5-1% of women who undergo CVS.
Complications
General: Complications of Alström syndrome affect many organs in the body. Alström syndrome may cause diabetes, obesity, heart problems, kidney disease, and lung problems, and other complications.
Developmental delays: About 20% of affected individuals have delays in early developmental milestones, such as gross and fine motor skills and in expressive and receptive language; about 30% have a learning disability. Severe intellectual disability, characterized by an IQ under 70, is very rare. The presence of these developmental disabilities may require specialized programs in school.
Diabetes complications: Diabetes is linked with long-term complications that affect almost every part of the body. The disease affects many Alström patients and often leads to blindness, heart and blood vessel disease, stroke, kidney failure, amputations, and nerve damage. Uncontrolled diabetes may complicate pregnancy, and birth defects are more common in babies born to women with diabetes. Pregnant women may temporarily develop gestational diabetes, a type of diabetes that begins late in pregnancy.
Hearing loss: Up to 70% of people with Alström syndrome gradually lose hearing during the first decade of life. By age 20, hearing loss may be classified as severe or moderately severe. Individuals with hearing loss need to learn how to communicate with people in other ways, including the use of sign language.
Heart problems: Individuals with Alström syndrome may develop a condition called cardiomyopathy, in which the muscular walls of the heart weaken. In dilated cardiomyopathy, the heart is not able to pump blood efficiently. Symptoms may include irregular heartbeat, fatigue, and shortness of breath.
Kidney disease: Some people with Alström syndrome may develop kidney disease, which may progress to life-threatening kidney failure if not treated properly.
Liver problems: Liver problems may be present in people with Alström syndrome. Hepatomegaly (an enlarged liver) and related complications may be life threatening. These include portal hypertension (high blood pressure in the vein that carries blood from the digestive tract to the liver) and may result in ascites (fluid in the abdominal cavity), splenomegaly (an enlarged spleen), and esophageal varices (extremely dilated veins in the esophagus).
Lung problems: Individuals with Alström syndrome may develop lung problems, which may include susceptibility to bronchitis and pulmonary hypertension (high blood pressure that affects the arteries in the lungs).
Obesity: Individuals with Alström syndrome typically develop obesity in early adulthood. Complications of obesity include high blood pressure, diabetes, and elevated cholesterol.
Pancreatitis: People with Alström syndrome may have high levels of triglycerides and total cholesterol in the blood. Very high levels of triglycerides have been associated with pancreatitis (inflammation of the pancreas) in individuals with Alström syndrome.
Treatment
General: There is no cure for Alström syndrome. Instead, treatment aims to reduce symptoms and prevent complications. Permanent blindness, deafness, and type 2 diabetes are likely to develop. Kidney and liver failure may worsen.
Corrective lenses: Eyeglasses are limited in their ability to improve vision in those with Alström syndrome. Tinted lenses may help with sensitivity to bright light. Because almost all people with Alström syndrome progressively lose vision, they should be instructed in the use of Braille, adaptive equipment, mobility aids, and adaptive computing skills early in life.
Education: By law, patients with Alström syndrome who suffer from intellectual disabilities must have access to education that is tailored to their specific strengths and weaknesses. According to the Individuals with Disabilities Education Act, all children with disabilities must receive free and appropriate education. Staff members of the patient's school must consult with the patient's parents or caregivers to design and write an individualized education plan based on the child's needs. The school faculty must document the child's progress in order to ensure that the child's needs are being met.
Educational programs vary among patients depending on the child's specific learning disabilities. In general, most experts believe that children with disabilities should be educated alongside their nondisabled peers. The idea is that nondisabled students will help the patient learn appropriate behavioral, social, and language skills. Therefore, some Alström syndrome patients are educated in mainstream classrooms. Others attend public schools but take special education classes. Still others attend specialized schools equipped to teach children with disabilities.
Hearing aids: People with Alström syndrome who experience hearing loss may benefit from hearing aids. These battery-operated devices are available in three basic styles: behind the ear, in the ear, and inside the ear canal. Patients should talk to a healthcare provider to determine the type of hearing aid that is best for them. A behind-the-ear device is used for mild-to-profound hearing loss. The device is worn behind the ear and is attached to a plastic ear mold inside the outer ear. In-the-ear hearing aids are worn inside the outer ear and are used for mild-to-severe hearing loss. Canal hearing aids are smaller hearing aids that fit inside the patient's ear canal. These are used for mild to moderately severe hearing loss. If hearing loss is severe, patients may benefit from cochlear implants. These electronic devices are surgically implanted inside the ears. Unlike a hearing aid, which amplifies sound, a cochlear implant compensates for damaged parts of the inner ear.
Diet: Consuming a healthful and appropriate diet is essential to people with Alström syndrome, because it may help minimize obesity and diabetes. The progression of diabetes may be slowed by consuming a diet limited in sugars and high in vegetables, whole grains, and lean protein. In fact, diet and exercise are often the first line of treatment for diabetes. An optimal diet for an individual with diabetes maybe planned with a registered dietitian (RD) or certified diabetes educator (CDE).
Occupational therapy: Patients with Alström syndrome may benefit from occupational therapy. During sessions, a therapist helps the child learn skills to help him or her perform basic daily tasks, such as eating, getting dressed, and communicating with others. Some patients work with therapists who specialize in disorders and disabilities. Parents and caregivers may ask their child's pediatrician for recommended therapists.
Physical activity: People with Alström syndrome should follow a regular plan of physical activity that is created with the help of a qualified healthcare provider such as a physician. Exercise not only reduces obesity but also helps control blood sugar levels.
Antibiotics: Some people with Alström syndrome who have lung problems are prone to infections such as bronchitis. To treat these infections, patients may be given antibiotics.
Oral diabetes medications: Many different types of drugs may be taken by mouth to treat diabetes. Some of these drugs may be combined into a single pill, which may be more effective and convenient for people with diabetes. Sulfonylureas such as chlorpropamide (Diabinese®), glipizide (Glucotrol®), glyburide (Micronase®, Glynase®, DiaBeta®), and glimepiride (Amaryl®) work by stimulating the cells of the pancreas to release more insulin. These drugs are taken once or twice daily by mouth before meals. Side effects may include an unsafe drop in blood sugar.
Meglitinides such as repaglinide (Prandin®) and nateglinide (Starlix®) also stimulate the cells of the pancreas to release more insulin. These drugs are taken by mouth before each meal and may also cause an unsafe drop in blood sugar. Side effects include weight gain and low blood sugar.
Metformin (Glucophage®) is a biguanide, a drug used to treat diabetes by decreasing the amount of blood sugar released by the liver and by stimulating cells in the muscles to take up blood sugar. Metformin is usually taken twice daily and may cause stomach upset. The most common side effect is diarrhea and acid reflux, occurring in up to 30% of patients.
Thiazolidinediones such as rosiglitazone (Avandia®) and pioglitazone (Actos®) help insulin work more efficiently in muscle and fat cells and cause the liver to release less glucose. These drugs may be associated with heart failure, and their use should be thoroughly discussed with a qualified healthcare provider, including a pharmacist.
Dipeptidyl peptidase IV (DPP-4) inhibitors such as sitagliptin (Januvia®) improve levels of blood sugar by decreasing the action of an enzyme that breaks down GLP-1, a substance that naturally lowers blood sugar levels. Alpha-glucosidase inhibitors such as acarbose (Precose®) and miglitol (Glyset®) block the breakdown of certain carbohydrates so they can be excreted. Side effects include intestinal gas and diarrhea.
Injected diabetes medications: Other diabetes drugs may be taken by injection into the fat just below the skin, called subcutaneous injection.
Pramlintide (Symlin®) is a synthetic form of insulin, a hormone that naturally occurs in the human body and serves to take up extra blood glucose. This drug, taken with meals, helps maintain normal levels of blood sugar. Side effects may include nausea.
Exenatide (Byetta®) is a synthetic form of exendin-4, a substance that naturally occurs in the body and helps increase insulin secretion from the pancreas. Side effects may include nausea, but this usually decreases with continued use of the drug.
Depending on the type and severity of diabetes, insulin may be introduced by subcutaneous injection. Insulin allows the body to use the sugar in the blood for energy. There are many different types of insulin, and a treatment strategy may be tailored to an individual patient's needs. Use of insulin therapy should be thoroughly discussed with a qualified healthcare provider and a certified diabetes educator (CDE).
Cholesterol-lowering drugs: Drugs that lower cholesterol and triglyceride levels may be necessary in some people with Alström syndrome. HMG-CoA reductase inhibitors, also called "statins," effectively lower levels of low-density lipoprotein (LDL, or "bad") cholesterol and triglycerides. High-dose nicotinic acid (niacin) may also reduce cholesterol levels.
Heart medications: Angiotensin-converting enzyme (ACE) inhibitors, diuretics, digoxin, and beta-blockers may help with the management of cardiomyopathy and heart failure.
Dialysis: When the kidneys begin to fail, patients may undergo several types of dialysis to restore their filtering function. In hemodialysis, a patient's blood is circulated into an external filter and cleaned. The filtered blood is then returned to the body. In peritoneal dialysis, a fluid containing dextrose is introduced into the abdomen through a tube. This solution absorbs the wastes in the body and is then removed.
Transplantation: Some patients who experience kidney failure may undergo kidney transplantation. Transplantation is associated with complications, including infection and the possibility of rejection of the new organ. To reduce the chance of rejection, patients may need to take immunosuppressive drugs.
Surgery: If scoliosis (sideways curvature of the spine) or kyphosis (forward curvature of the spine) is severe, surgery may be required.
Integrative Therapies
Currently there is limited scientific evidence on the use of integrative therapies for the treatment or prevention of Alström syndrome.
Prevention
General: Alström syndrome is an inherited condition, or passed down among family members. Therefore, there is currently no known way to prevent the disease. However, a number of options are available for prospective parents with a family history of Alström syndrome.
Genetic testing and counseling: Individuals who have Alström syndrome may meet with a genetic counselor to discuss the risks of having children with the disease. Individuals with a family history of Alström syndrome may meet with a genetic counselor to determine whether they carry the defective ALMS1 gene. Carriers can be determined through detailed family histories or genetic testing.
Known carriers of Alström syndrome may undergo genetic counseling before they conceive a child. Genetic counselors may explain the options and the associated risks of various tests, including preimplantation genetic diagnosis (PGD), amniocentesis, and chorionic villus sampling (CVS).
PGD may be used with in vitro (artificial) fertilization. In PGD, embryos are tested for the defective ALMS1 gene, and only the embryos that are not affected may be selected for implantation. Because Alström syndrome may be detected in a fetus, parents may choose whether to continue the pregnancy. Genetic counselors may assist parents with these difficult decisions.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
American Society for Deaf Children. www.deafchildren.org.
Bond J, Flintoff K, Higgins J, et al. The importance of seeking ALMS1 mutations in infants with dilated cardiomyopathy. J Med Genet. 2005; 42: e10. View Abstract
Cardiomyopathy Association. www.cardiomyopathy.org.
Children's Cardiomyopathy Foundation (CCF). www.childrenscardiomyopathy.org.
Collin GB, Marshall JD, Ikeda A, et al. Mutations in ALMS1 cause obesity, type 2 diabetes and neurosensory degeneration in Alstrom syndrome. Nat Genet. 2002; 31: 74-8. View Abstract
Deeble VJ, Roberts E, Jackson A, et al. The continuing failure to recognise Alstrom syndrome and further evidence of genetic homogeneity. J Med Genet. 2000; 37: 219. View Abstract
Maffei P, Boschetti M, Marshall JD, et al. Characterization of the IGF system in 15 patients with Alstrom syndrome. Clin Endocrinol (Oxf). 2007; 66: 269-75. View Abstract
Maffei P, Munno V, Marshall JD, et al. The Alstrom syndrome: is it a rare or unknown disease? Ann Ital Med Int. 2002; 17: 221-8. View Abstract
Makaryus AN, Popkowski B, Kort S, et al. A rare case of Alstrom syndrome presenting with rapidly progressive severe dilated cardiomyopathy diagnosed by echocardiography. J Am Soc Echocardiography. 2003; 16: 194-6. View Abstract
Marshall JD, Bronson RT, Collin GB, et al. New Alstrom syndrome phenotypes based on the evaluation of 182 cases. Arch Intern Med. 2005; 165: 675-83. View Abstract
Michaud JL, Heon E, Guilbert F, et al. Natural history of Alstrom syndrome in early childhood: onset with dilated cardiomyopathy. J Pediatr. 1996; 128: 225-9. View Abstract
Minton JA, Owen KR, Ricketts CJ, et al. Syndromic obesity and diabetes: changes in body composition with age and mutation analysis of ALMS1 in 12 United Kingdom kindreds with Alstrom syndrome. J Clin Endocrinol Metab. 2006; 91: 3110-6. View Abstract
National Eye Institute. www.nei.nih.gov.
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Quiros-Tejeira RE, Vargas J, Ament ME. Early-onset liver disease complicated with acute liver failure in Alstrom syndrome. Am J Med Genet. 2001; 101: 9-11. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017